Acitretin Pregnancy Risk Calculator
Acitretin can cause birth defects for up to 3 years after you stop taking it. This tool helps you calculate the safe window for pregnancy after stopping the medication.
Important Safety Information
Acitretin remains in your body as a metabolite for up to 3 years after stopping. Do not attempt pregnancy during this time period.
Your safe pregnancy window starts . We strongly recommend using two forms of contraception throughout the entire 3-year period.
Recommendation
Do not attempt pregnancy until . We recommend continuing contraception for the full 3-year window after stopping Acitretin.
Warning: This tool provides general guidance only. Please consult with your healthcare provider for personalized medical advice regarding pregnancy and medication safety.
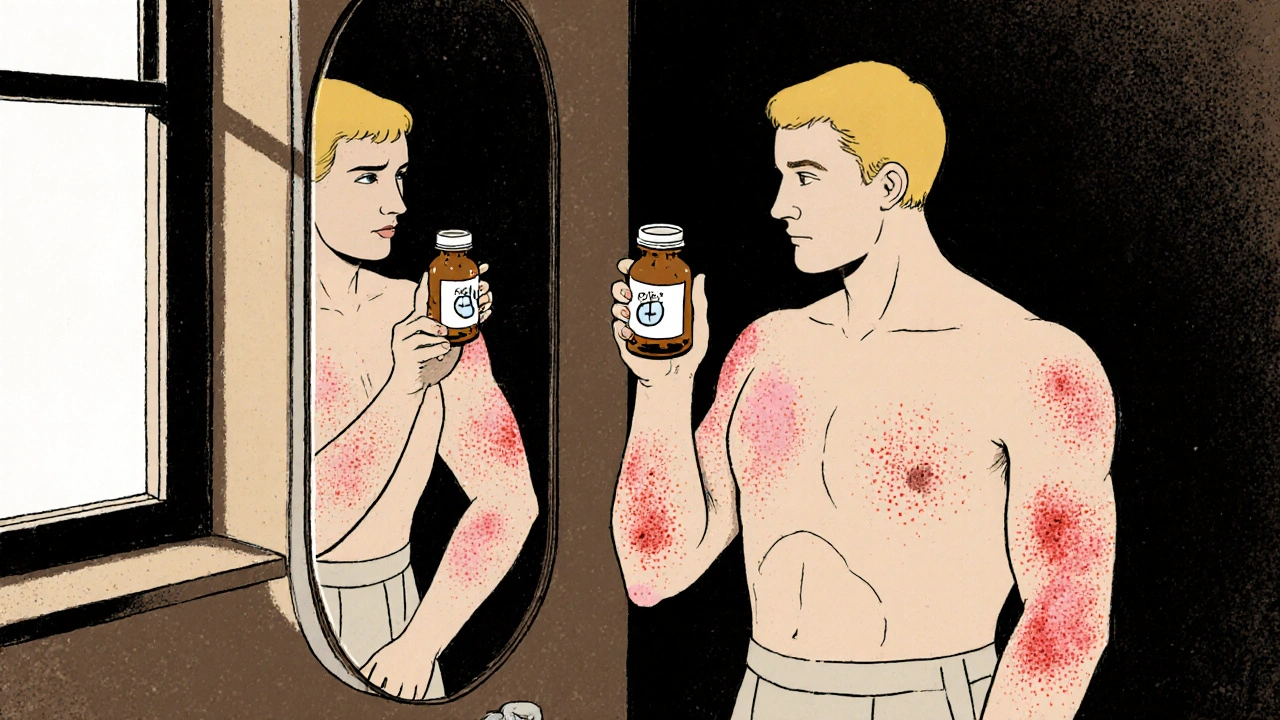
If you or someone you know has been prescribed Acitretin is an oral retinoid used for severe plaque psoriasis is a chronic skin condition that causes thick, red patches. While the drug can clear stubborn lesions, it also brings a mix of bite‑size annoyances and serious warnings. This guide walks through the most common complaints, the red‑flag risks, who should stay clear, and practical ways to keep the side‑effects in check.
Quick Takeaways
- Acitretin side effects range from dry skin and lips to liver‑related issues.
- Pregnancy contraindication is absolute - teratogenic risk lasts up to three years after stopping.
- Regular blood work (liver enzymes, lipids, bone health) is non‑negotiable.
- Hydration, moisturizers, and diet tweaks can blunt many mild symptoms.
- Alternative systemic options include Isotretinoin (another retinoid) and Methotrexate (an immunosuppressant).
How Acitretin Works
Acitretin is a synthetic analog of vitamin A. It binds to nuclear retinoic‑acid receptors, prompting skin cells to differentiate normally and reducing the over‑production of keratin. The result is slower turnover and less scaling. Because the mechanism targets the skin directly, the drug avoids some of the immune‑modulating side‑effects seen with biologics, but it also interferes with other vitamin‑A‑dependent processes in the liver, bone, and lipid metabolism.
Common Side Effects You’ll Notice
Most patients report at least one of the following within the first few weeks:
- Dry skin, lips, and nails - the classic retinoid “dry‑ness” that can feel like a winter‑time flare.
- Hair thinning - especially on the scalp; it’s usually reversible after stopping.
- Elevated triglycerides - blood tests often show a 20‑30 % rise; diet can help.
- Headache or mild joint aches - likely tied to changes in bone turnover.
- Cheilitis (cracked lips) - the most visible complaint, often managed with a good lip balm.
These issues are bothersome but manageable for most people. Staying ahead with moisturizers, water intake, and occasional labs can keep them from becoming a deal‑breaker.
Serious Risks You Can’t Ignore
While the mild complaints are annoying, a handful of serious risks demand vigilance:
- Liver toxicity is the most frequent lab abnormality. Elevated ALT/AST can appear in 5‑10 % of users; severe hepatitis is rare but possible.
- Hyperlipidemia - triglycerides can climb above 500 mg/dL in vulnerable patients, increasing pancreatitis risk.
- Teratogenicity is a headline warning. Even low doses can cause birth defects; the drug stays in the body as a metabolite for up to three years.
- Bone demineralization - long‑term use may lower bone density, especially in post‑menopausal women.
- Severe allergic reactions (rare) - rash, swelling, or respiratory distress need immediate medical attention.
Because of these risks, physicians order baseline and follow‑up labs at 4‑6 week intervals for the first 3 months, then every 2‑3 months thereafter.
Who Should Avoid Acitretin
The drug is contraindicated for:
- Anyone who is pregnant, planning pregnancy, or could become pregnant without reliable contraception.
- Patients with active liver disease or unexplained persistent elevations in liver enzymes.
- Those with uncontrolled hyperlipidemia (triglycerides > 400 mg/dL) unless diet/meds can bring them down.
- Individuals with severe osteoporosis or a history of fractures.
- Children under 12 years old - safety data are limited.
If any of these apply, doctors typically pivot to a biologic (e.g., TNF‑α inhibitor) or a different systemic such as methotrexate.
Managing Side Effects: Tips and Tricks
- Moisturize aggressively: Use ointments (petrolatum‑based) rather than lotions; apply right after showering.
- Lip care: Keep a flavored, fragrance‑free balm handy; reapply every hour during dry weather.
- Hydration: Aim for at least 2 L of water daily to help skin retain moisture.
- Diet for lipids: Limit sugary drinks, fried foods, and alcohol; add omega‑3 rich fish or flaxseed.
- Sun protection: Acitretin increases photosensitivity; use SPF 30+ broad‑spectrum sunscreen.
- Regular labs: Track ALT, AST, bilirubin, triglycerides, cholesterol, and calcium‑phosphate balance.
- Bone health: Vitamin D and calcium supplements, plus weight‑bearing exercise, can offset demineralization.
- Contraception: Use two reliable methods (e.g., hormonal IUD + condom) for the full three‑year window after stopping.
If side effects become intolerable, discuss dose reduction or a switch with your dermatologist.

Acitretin Compared to Other Systemic Psoriasis Drugs
| Drug | Primary Indication | Mechanism | Typical Dose | Common Side Effects | Pregnancy Contraindication |
|---|---|---|---|---|---|
| Acitretin | Severe plaque psoriasis | Oral retinoid - binds RAR/RXR receptors | 25‑50 mg daily | Dry skin, elevated triglycerides, liver enzyme rise | Yes - teratogenic up to 3 years |
| Isotretinoin | Severe acne; off‑label psoriasis | Oral retinoid - similar to acitretin | 0.5‑1 mg/kg/day | Dry mucosa, mood changes, liver changes | Yes - strict iPLEDGE program |
| Methotrexate | Psoriasis, rheumatoid arthritis | Folate antagonist - inhibits DNA synthesis | 7.5‑25 mg weekly | Nausea, hepatic fibrosis, bone marrow suppression | No - but must avoid pregnancy during treatment and 3 months after |
Choosing the right drug hinges on factors like age, reproductive plans, liver health, and how quickly you need clearance. Acitretin shines for patients who can’t take biologics and need a non‑immunosuppressive option, but the pregnancy rule is a deal‑breaker for many.
Bottom Line Checklist
- Confirm baseline liver enzymes, lipid panel, and pregnancy test.
- Start with the lowest effective dose; titrate up slowly.
- Track side‑effects daily - especially skin dryness and any abdominal pain.
- Schedule labs at weeks 4, 8, 12, then every 2‑3 months.
- Maintain strict contraception for the full three‑year post‑treatment window.
- Consider switching if triglycerides > 500 mg/dL or ALT/AST > 3× ULN.
Frequently Asked Questions
Can I drink alcohol while on acitretin?
Alcohol can worsen liver enzyme elevation and raise triglycerides. If you choose to drink, keep it occasional and under low‑risk limits (no more than 1‑2 drinks per week) and monitor labs closely.
How long does it take to see skin improvement?
Most patients notice a reduction in plaque thickness after 8‑12 weeks, though full clearance can take 4‑6 months of consistent dosing.
Is acitretin safe for long‑term use?
Long‑term use is possible but requires ongoing monitoring of liver function, lipids, and bone density. Many clinicians limit continuous therapy to 12‑18 months and then pause.
What should I do if I get a severe rash?
Stop the medication immediately and contact your dermatologist. Severe rashes could signal a hypersensitivity reaction that needs urgent evaluation.
Can acitretin be used together with biologics?
Combining two systemic agents increases toxicity risk and isn’t routinely recommended. Some specialists may overlap for a short bridge period, but that should be done only under close supervision.

laura wood
October 20, 2025 AT 17:45Staying hydrated and using a thick ointment can really soften the dry skin that acitretin brings.
Kate McKay
October 29, 2025 AT 22:58When you start acitretin, the first thing to do is to stock up on a good, petrolatum‑based moisturizer and apply it right after showering; this creates a barrier that keeps the skin from losing too much water.
Don’t forget to keep a fragrance‑free lip balm handy and reapply it frequently, especially in dry environments.
Drinking at least two liters of water a day will help your skin stay supple and can also ease the dry‑mouth sensation that sometimes accompanies retinoids.
Regular blood work for liver enzymes and triglycerides is non‑negotiable, so set reminders on your phone to keep the appointments.
And finally, if you notice any sudden joint pain or extreme fatigue, bring it up with your dermatologist right away – early intervention can prevent larger problems down the line.
Demetri Huyler
November 8, 2025 AT 05:12Look, the United States has some of the best dermatology research out there, so when a doctor prescribes acitretin you can trust that it’s backed by solid clinical data.
That said, the drug isn’t a free‑for‑all; you have to respect the strict monitoring protocols, otherwise you’re just flirting with unnecessary risk.
Our labs are usually done at four‑week intervals, and the results are reviewed by board‑certified specialists who know exactly what counts as a red flag.
People who skimp on these tests often end up with avoidable liver issues or sky‑high triglycerides, which could have been caught early.
And let’s be clear: the teratogenic warning isn’t a suggestion – it’s an absolute rule that reflects decades of hard‑won experience.
If you’re serious about your health, follow the guidelines and you’ll see why American dermatology remains a global leader.
JessicaAnn Sutton
November 17, 2025 AT 11:25Acitretin’s teratogenic profile demands the highest ethical standards from both prescribers and patients, as the potential for severe congenital malformations is unequivocal. The pharmacokinetic persistence of its active metabolite for up to three years post‑cessation imposes a lifelong responsibility to maintain reliable contraception, a duty that cannot be overstated. Moreover, the moral imperative to conduct baseline liver function testing before initiating therapy is rooted in the well‑documented incidence of hepatic enzyme elevations in a non‑trivial subset of users. Regular monitoring of triglyceride levels is equally compulsory, given the drug’s capacity to precipitate hyperlipidemia that may culminate in acute pancreatitis. Bone health assessments, including dual‑energy X‑ray absorptiometry, should be scheduled at six‑month intervals for patients on prolonged courses, as osteopenia has been reported in longitudinal studies. In addition, clinicians must counsel patients on the unequivocal contraindication for pregnancy, emphasizing that even low‑dose exposure can result in fetal anomalies such as craniofacial defects and limb malformations. The principle of “do no harm” obliges physicians to weigh these risks against the therapeutic benefits, particularly when alternative systemic agents with more favorable safety profiles are available. From an ethical standpoint, informed consent must explicitly detail the magnitude of these risks, ensuring that patients are not merely passive recipients of a prescription but active participants in their care plan. The healthcare system should also provide access to reliable contraception methods, recognizing that socioeconomic barriers can inadvertently compromise compliance. Furthermore, patients should be educated on recognizing early warning signs of liver toxicity, such as jaundice, pruritus, or unexplained fatigue, and instructed to seek immediate medical attention should these occur. In the event of severe adverse reactions, prompt discontinuation of acitretin is essential, followed by a comprehensive evaluation to mitigate lingering effects. The cumulative evidence underscores the necessity for a multidisciplinary approach, integrating dermatology, hepatology, and endocrinology expertise when managing complex cases. Finally, ongoing research into pharmacogenomic predictors of adverse outcomes may eventually refine patient selection, reducing reliance on blanket contraindications. Until such advances are realized, the prudent course remains rigorous adherence to established monitoring protocols and unwavering commitment to patient education. Patients and providers alike must remain vigilant, as the balance between efficacy and safety is a dynamic equation that evolves with each new clinical observation.
Israel Emory
November 26, 2025 AT 17:38When you’re on acitretin, remember to schedule your labs, keep a diary of any skin changes, note any headaches, and report joint aches, because early detection, indeed, can prevent complications, and the dermatologist will appreciate the thoroughness.
Hydration, moisturization, and sunscreen application should become daily rituals, not optional add‑ons, as the drug heightens photosensitivity, and neglect can exacerbate erythema.
If you’re planning a pregnancy, double‑check your contraception, discuss with your provider, and never assume a short washout period is sufficient, since the metabolite persists for years.
Sebastian Green
December 5, 2025 AT 23:52I’ve been there, and the dry lips can feel like you’re constantly walking on sand; keep a fragrance‑free balm nearby and reapply often, it really makes a difference.
Wesley Humble
December 15, 2025 AT 06:05It is imperative to adhere to the monitoring schedule, as deviations may result in hepatic decompensation; please ensure that ALT and AST values remain within the reference range, and consider a lipid panel every six weeks. 🙂 Additionally, the teratogenic risk obligates the use of two reliable contraceptive methods, a recommendation supported by multiple epidemiological studies. 🙂 Should any adverse reaction such as severe rash occur, immediate discontinuation and consultation with a specialist are warranted. 🙂 Maintaining a detailed log of symptoms can facilitate prompt clinical decisions.
barnabas jacob
December 24, 2025 AT 12:18Yo, the retinoid pathway triggers keratinocyte differentiation, but you’ll also see a spike in serum TGs – that’s hyperlipidemia 101, bro.
Don’t slipp on the labs, cuz the liver enzymes can go sideways fast.
Stick to a low‑carb diet, load up on omega‑3s, and keep the moisturizers on lock.
Kirsten Youtsey
January 2, 2026 AT 18:32The pharmaceutical narrative surrounding acitretin often downplays the long‑term skeletal implications, a fact that becomes evident when independent studies reveal a statistically significant reduction in bone mineral density after extended therapy. One must therefore question whether the regulatory oversight truly safeguards patient welfare or merely serves corporate interests. The necessity for dual‑method contraception for three years post‑treatment is presented as a precaution, yet the underlying motive may be to extend market dominance by limiting alternative therapeutic avenues. Moreover, the omission of comprehensive risk‑benefit analyses in public prescribing guidelines suggests a systemic bias that favors profit over transparency. Clinicians are urged to scrutinize the primary literature, demand full disclosure from manufacturers, and consider non‑retinoid options when feasible.
jessie cole
January 12, 2026 AT 00:45Remember, perseverance in managing side‑effects is a testament to your commitment to health; each moisturized night and each lab result represents progress.
Do not let occasional dryness undermine the ultimate goal of clearer skin, for the journey, though arduous, yields lasting rewards.
Stay vigilant, stay hopeful, and trust that your dermatologist’s guidance, when followed diligently, will steer you toward success.
Matthew Hall
January 21, 2026 AT 06:58Man, I thought I could handle acitretin like a champ, but the lips were cracking like old paint!
Every time I looked in the mirror, the dry patches stared back, and I was like, “Seriously??”
Turns out I wasn’t drinking enough water, and the moisturizer I used was just a light lotion – total fail.
After I switched to a thick ointment and set alarms to chug water, the skin finally started to calm down.
Now I’m keeping a journal, and honestly, it feels like I’ve won a small war against the side‑effects.
Vijaypal Yadav
January 30, 2026 AT 13:12To augment the monitoring protocol outlined earlier, consider adding a baseline vitamin D level and a repeat DEXA scan after twelve months of continuous therapy; studies indicate that acitretin can modestly accelerate cortical bone loss, especially in post‑menopausal individuals. Moreover, a fasting lipid panel that includes HDL, LDL, and triglycerides provides a more comprehensive view than triglycerides alone, allowing for earlier dietary or pharmacologic intervention. It is also advisable to schedule a brief hepatic ultrasound if ALT/AST elevations exceed three times the upper limit, as this can help differentiate drug‑induced injury from underlying structural pathology.