Antibiotic Liver Injury Calculator
Liver Injury Calculator
Calculate the R-ratio to identify the type of antibiotic-related liver injury based on your lab results.
Results
Enter your lab values to see the calculation results
Antibiotics save lives. But for some people, the very drugs meant to fight infection can quietly damage the liver - sometimes without warning. It’s not rare. In fact, antibiotics cause 64% of all drug-induced liver injuries in ICU patients. That’s more than any other class of medication. And while most people take them without issue, a small but significant number develop hepatitis (liver inflammation) or cholestasis (bile flow blockage) as a side effect. Understanding how this happens, who’s at risk, and what to watch for can make all the difference.
How Antibiotics Hurt the Liver
It’s not just one way antibiotics damage the liver. They trigger multiple pathways. One major mechanism is mitochondrial dysfunction. Antibiotics like amoxicillin-clavulanate and tazobactam/piperacillin interfere with the energy factories inside liver cells. This leads to a buildup of toxic byproducts, oxidative stress, and eventually cell death. Another key player is the gut microbiome. Antibiotics wipe out good bacteria, allowing harmful ones to take over. This disrupts the gut barrier, letting toxins leak into the bloodstream and reach the liver - a process called endotoxemia. The liver then gets overwhelmed trying to filter them out.
Some antibiotics form reactive metabolites - unstable chemical fragments - that bind directly to liver proteins. This tricks the immune system into attacking the liver, even after the drug is gone. Genetic factors also matter. Certain HLA gene variants make some people far more susceptible. If you’ve had a bad reaction to one antibiotic, your chances of reacting to another are higher.
Hepatitis vs. Cholestasis: The Two Faces of Injury
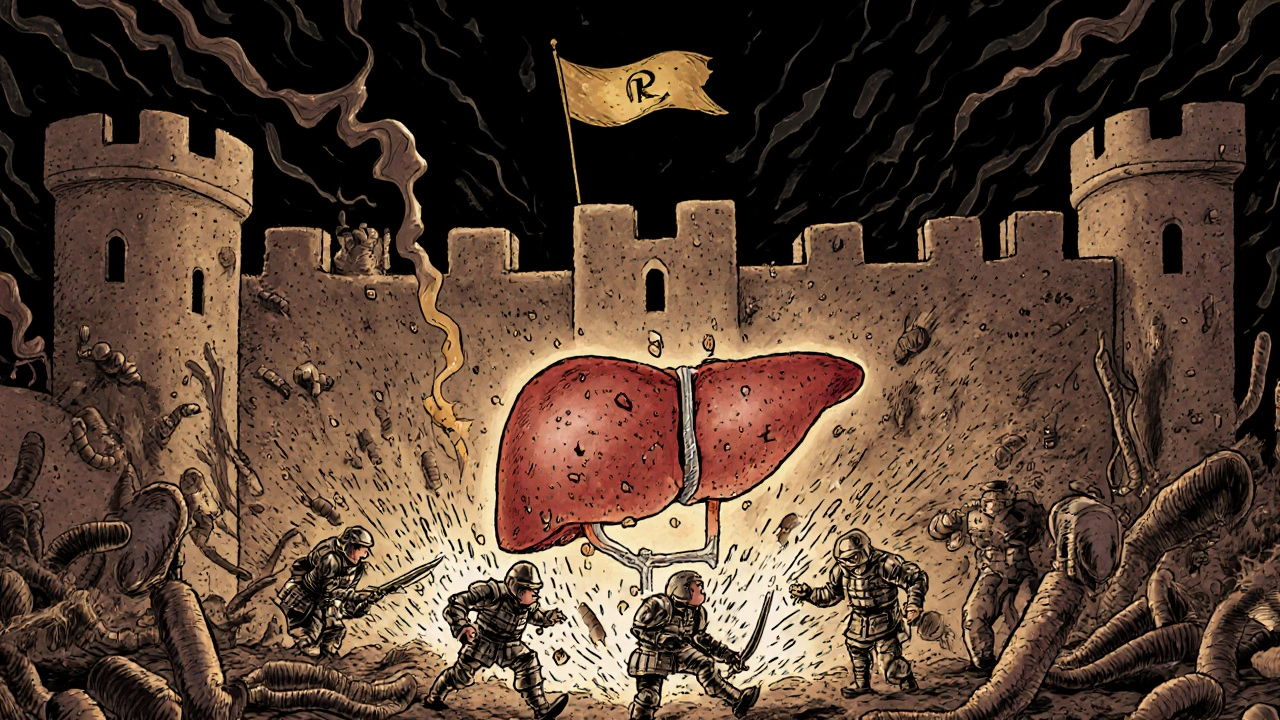
Not all liver damage from antibiotics looks the same. Doctors classify it using something called the R-ratio. It’s a simple calculation: (ALT level / ULN) divided by (ALP level / ULN). This tells you whether the injury is mostly liver cell damage (hepatitis) or bile flow blockage (cholestasis).
- Hepatocellular injury (hepatitis): ALT rises more than ALP. R-ratio > 5. Think of it as the liver cells themselves being burned out. Common with ciprofloxacin and azithromycin.
- Cholestatic injury: ALP rises more than ALT. R-ratio < 2. Bile isn’t flowing right. Amoxicillin-clavulanate is the classic culprit - 70-80% of its liver injuries are cholestatic.
- Mixed injury: R-ratio between 2 and 5. Both patterns show up. Often seen with prolonged antibiotic use.
Lab numbers matter. Hepatocellular injury is defined as ALT more than 5 times the upper limit of normal. Cholestasis is ALP more than 2 times normal. If bilirubin also spikes above 2 times normal, that’s a red flag for serious injury.
Which Antibiotics Are the Biggest Risks?
Some antibiotics are far more likely to cause liver damage than others. The data is clear.
| Antibiotic | Typical Injury Pattern | Incidence per 100,000 Prescriptions | Time to Onset |
|---|---|---|---|
| Amoxicillin-clavulanate | Cholestatic | 15-20 | 1-6 weeks |
| Tazobactam/piperacillin (TZP) | Mixed | 28.7% in ICU (≥7 days) | 1-3 weeks |
| Ciprofloxacin | Mixed | 1-3 | 1-2 weeks |
| Azithromycin | Mixed | 1-3 | 1-4 weeks |
| Rifampin | Hepatocellular | 5-10 | 2-8 weeks |
| Nitrofurantoin | Mixed | 2-5 | 1-4 weeks |
Amoxicillin-clavulanate tops the list. It’s one of the most commonly prescribed antibiotics - and one of the most dangerous for the liver. In ICU settings, tazobactam/piperacillin is even more concerning. One study found nearly 3 out of 10 patients on this combo for over a week developed liver injury. And men are 2.4 times more likely than women to suffer liver damage from meropenem.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop antibiotic-related liver injury.
- People on antibiotics for 7+ days: The risk jumps 3.2 times compared to shorter courses.
- ICU patients: They often get multiple antibiotics, have sepsis, and are already stressed. Sepsis alone increases liver injury risk by 1.8 times.
- Older adults: Liver metabolism slows with age. Detox pathways aren’t as efficient.
- People with pre-existing liver disease: Even mild fatty liver can make things worse.
- Those with specific HLA genes: Genetic testing isn’t routine yet - but research is moving fast.
Women are more likely to get cholestatic injury. Men are more likely to get hepatocellular injury - especially with meropenem. And if you’ve had a previous drug reaction, your odds go up again.
What Symptoms Should You Watch For?
Many people have no symptoms at all. Their liver enzymes just creep up on a routine blood test. But when symptoms do appear, they can be subtle - or severe.
- Unexplained fatigue
- Loss of appetite
- Nausea or vomiting
- Dark urine
- Light-colored stools
- Yellowing of skin or eyes (jaundice)
- Itchy skin (especially in cholestasis)
These signs don’t always mean it’s the antibiotic. In the ICU, patients often have sepsis, low blood pressure, or other liver problems. That’s why it’s so hard to tell what’s causing the damage. But if you’re on an antibiotic and start feeling worse - especially with jaundice - tell your doctor right away.
How Doctors Diagnose and Monitor It
There’s no single test. Diagnosis is about ruling out other causes and connecting the dots.
Before starting a high-risk antibiotic like amoxicillin-clavulanate or TZP, doctors should check baseline liver tests. Then, repeat them after 1-2 weeks. For patients in the ICU on long-term antibiotics, weekly tests are standard.
The American Association for the Study of Liver Diseases recommends stopping the antibiotic if:
- ALT is more than 5 times the upper limit of normal, OR
- ALP is more than 2 times normal AND you have symptoms like jaundice or itching.
But rules aren’t absolute. If you have a life-threatening infection and no other antibiotics work, doctors might keep going - with closer monitoring. That’s why experience matters. Most clinicians need 6-12 months to reliably spot the difference between antibiotic injury and other liver problems.
What Happens After Stopping the Antibiotic?
Good news: in most cases, the liver heals on its own. Once the drug is stopped, enzymes usually start falling within days. Full recovery can take weeks to months.
But not everyone recovers fully. About 10-15% of cases progress to severe injury - including acute liver failure. That’s rare, but it happens. Amoxicillin-clavulanate is the most common cause of acute liver failure from antibiotics in the U.S.
There’s no antidote. No specific treatment. Supportive care is all there is: fluids, rest, avoiding alcohol and other liver stressors. In severe cases, a liver transplant may be the only option.
What’s New in Research and Treatment
Science is catching up. One exciting area is the gut microbiome. Researchers found that people with low levels of Faecalibacterium prausnitzii - a good gut bacterium - are 3.7 times more likely to develop antibiotic-related liver injury. That could lead to simple stool tests to predict risk before prescribing.
Clinical trials are testing probiotics to protect the gut during antibiotic treatment. Early results are promising. If they work, we might soon recommend a specific probiotic strain alongside high-risk antibiotics.
Genetic testing is another frontier. HLA markers linked to idiosyncratic reactions are being mapped. In 5-7 years, we may be able to screen patients before giving them certain antibiotics - especially those with family histories of drug reactions.
The FDA and EMA now require stronger warnings on labels for newer β-lactam/β-lactamase inhibitor combos. And drug companies are thinking twice before developing new antibiotics that show even mild signs of liver toxicity in early trials. DILI causes nearly 1 in 5 drug failures during development.
What You Can Do
If you’re prescribed an antibiotic:
- Ask: Is this the best choice? Are there lower-risk options?
- Know the signs of liver trouble - don’t wait for jaundice.
- Don’t skip follow-up blood tests - even if you feel fine.
- Keep a list of all medications, including supplements. Some herbs (like kava or green tea extract) can worsen liver stress.
- If you’ve had a bad reaction before, tell every doctor. Write it down in your medical records.
Antibiotics are essential. But they’re not harmless. The liver doesn’t scream when it’s hurt - it whispers. Pay attention to those whispers. Your liver will thank you.
Can antibiotics cause permanent liver damage?
In most cases, no. Liver function returns to normal after stopping the antibiotic. But in about 10-15% of severe cases, especially with amoxicillin-clavulanate, injury can progress to acute liver failure. If that happens, permanent damage or transplant may be needed. Early recognition is key to avoiding this.
Are over-the-counter antibiotics linked to liver injury?
In most countries, true antibiotics require a prescription. But some OTC products - like certain herbal supplements, weight-loss pills, or even high-dose vitamin A - can cause liver injury on their own. Never assume something is safe just because it’s available without a prescription. Always check with your doctor before mixing supplements with antibiotics.
How long after stopping an antibiotic does liver damage improve?
ALT and ALP levels usually begin dropping within 1-2 weeks of stopping the drug. Full recovery can take 4-12 weeks, depending on the severity. Jaundice and itching may take longer to resolve. If enzymes don’t improve after 4 weeks, further evaluation is needed.
Can I take antibiotics again if I had liver injury before?
Avoid the same antibiotic - and often similar ones in the same class. For example, if amoxicillin-clavulanate caused injury, avoid other penicillin/β-lactamase inhibitor combos. Your doctor may choose an alternative like doxycycline or a non-β-lactam option. Always inform every provider about your history.
Do probiotics help prevent antibiotic-related liver injury?
Emerging evidence suggests yes - especially for high-risk patients. Clinical trials are testing specific strains like Lactobacillus rhamnosus and Bifidobacterium infantis to restore gut balance during antibiotic use. While not yet standard practice, some doctors recommend them for patients on long-term or high-risk antibiotics. Talk to your provider about whether it’s right for you.

Nikki C
November 24, 2025 AT 11:22Been on amoxicillin-clavulanate twice. First time, I just felt off. Second time, my skin turned yellow. No warning. No screaming liver. Just... quiet failure. Now I ask for alternatives before they even write the script. Don't wait for jaundice. Listen to the whisper.
Jacob McConaghy
November 24, 2025 AT 12:11This is the kind of post that should be mandatory reading before you get any antibiotic, especially in the hospital. I work in ER and see way too many patients with liver enzymes through the roof because no one checked baseline labs. Docs get rushed. Patients assume antibiotics are harmless candy. We need better protocols-and better patient education. This isn't scare tactics. It's harm reduction.
Andy Louis-Charles
November 26, 2025 AT 00:56TL;DR: Antibiotics = silent liver assassin. 🚨
Amoxicillin-clavulanate = #1 culprit.
Get your LFTs checked before and after.
Probiotics might help.
Don't ignore fatigue or dark pee.
And yes, your grandma was right-don't take meds without asking questions.
Douglas cardoza
November 27, 2025 AT 21:37My dad got liver failure from TZP in the ICU. They didn't even monitor his enzymes until it was too late. He's fine now but had to get a transplant. This info saved my life. I made sure my docs know his history before they touch me with any beta-lactam. Seriously, if you're on antibiotics longer than a week-ask for a liver panel. It's a 5-minute blood draw.
Adam Hainsfurther
November 29, 2025 AT 02:28It's wild how little we talk about this. We warn about antibiotics and C. diff, but liver damage? Almost never mentioned. And yet, 64% of drug-induced liver injuries? That’s not a footnote. That’s the headline. Why isn’t this on the prescription label? Why isn’t every pharmacy giving out a one-pager? We treat antibiotics like aspirin. They’re not. They’re powerful tools with serious trade-offs.
Rachael Gallagher
November 29, 2025 AT 23:42Big Pharma doesn't want you to know this. They make billions off antibiotics and ignore the liver damage because it's 'rare.' But when it hits, it hits hard. And they'll still sell you the next one. Stay smart. Stay skeptical.
steven patiño palacio
November 30, 2025 AT 14:51Important clarification: The R-ratio is a useful tool, but it's not perfect. Some patients present with mixed patterns early on, and others develop cholestasis after initially showing hepatocellular injury. Monitoring trends over time matters more than a single value. Also, ALT and ALP thresholds vary slightly by lab-always check your lab’s reference range. Knowledge is power, but context is king.
stephanie Hill
December 2, 2025 AT 03:38Ever notice how every new antibiotic comes out with a tiny warning buried in 12-point font? And then the ads say 'safe and effective'? Yeah. They know. They just don't care. I’ve got a friend who got liver failure from azithromycin. She was told it was 'just a stomach bug.' Now she's on the transplant list. And the company? Still selling it like it’s yogurt. 😒