CK Level Interpreter for Statin Therapy
Enter your CK level and select your sex to see your results
Understanding CK Interpretation
CK levels vary between individuals. For men, the normal range is typically 145-195 U/L. For women, it's 65-110 U/L.
When you start statins, your doctor compares your current CK level to your baseline. An increase of 3x or more above your baseline is significant.
High CK levels don't always mean statin-related muscle damage—exercise, injections, or other factors can cause elevations too.
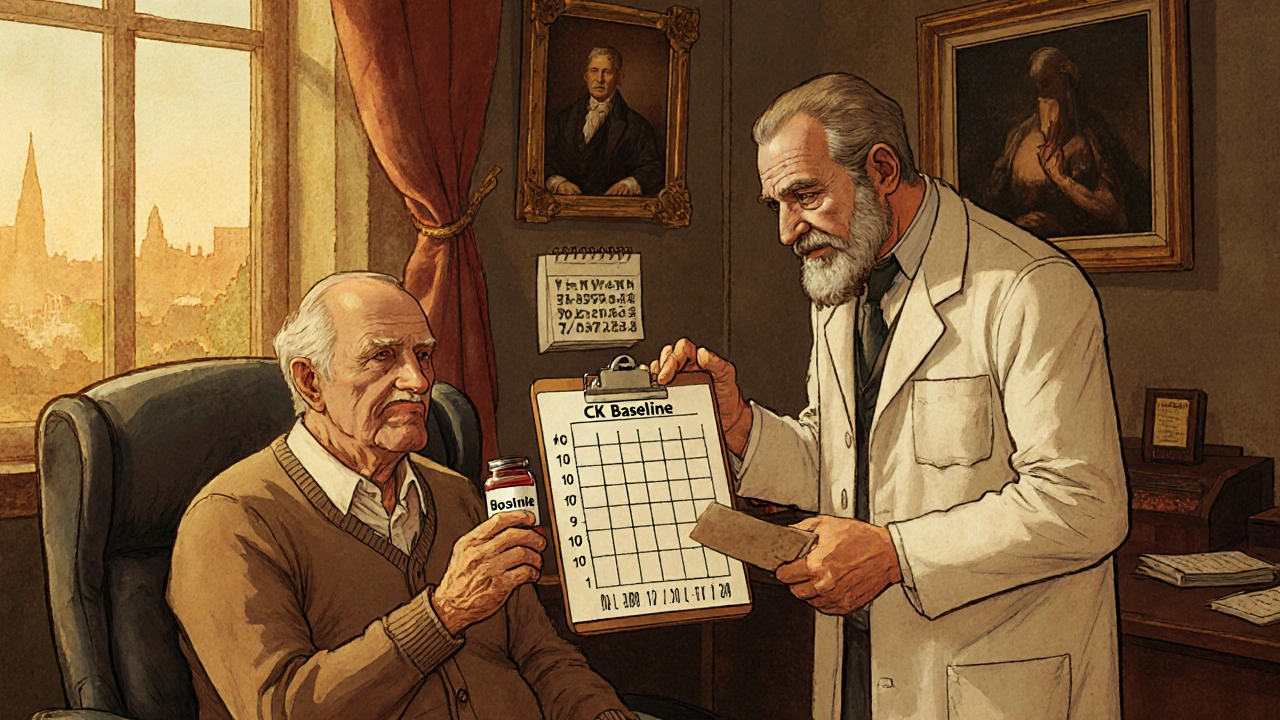
When you start a statin, your doctor might ask you to get a blood test for creatine kinase (CK) before you take your first pill. You might wonder: Why? Isn’t this just another lab test that adds cost and hassle? The truth is, baseline CK testing isn’t always necessary-but when it is, it can prevent big mistakes.
What Is CK, and Why Does It Matter with Statins?
Creatine kinase (CK) is an enzyme found in your muscles. When muscle cells get damaged, CK leaks into your bloodstream. High levels can mean something’s wrong-like a heart attack, a serious muscle injury, or, in rare cases, statin-induced muscle damage. Statin-related muscle problems range from mild aches (myalgia) to a life-threatening condition called rhabdomyolysis, where muscle tissue breaks down and can wreck your kidneys. While rhabdomyolysis is extremely rare-happening in about 0.1% of users-it’s the kind of thing you don’t want to miss. The problem? Many people feel muscle soreness after starting statins, but most of the time, it’s not actually caused by the drug. Studies show that 78% of patients who report muscle pain while on statins have CK levels that are normal or only slightly elevated. That means their pain likely comes from something else-overdoing it at the gym, arthritis, or just aging. That’s where baseline CK comes in. If you know what your normal CK level is before starting a statin, you can tell later whether any rise is real or just noise.Who Actually Needs a Baseline CK Test?
Not everyone. The American College of Cardiology and American Heart Association don’t recommend routine baseline CK for healthy people starting statins. But there are clear groups where it makes sense:- People over 75 years old
- Those with kidney problems (eGFR below 60)
- Patients with hypothyroidism (about 1 in 8 statin users have this)
- Anyone taking other drugs that interact with statins-like amiodarone, fibrates, or certain antibiotics
- People who had muscle issues with statins before
- Those on high-intensity statins (atorvastatin 40-80 mg or rosuvastatin 20-40 mg)
What Do the Numbers Mean?
CK levels vary wildly between people. A normal range for men is typically 145-195 U/L, and for women, 65-110 U/L. But that’s just a general guide. Some healthy people-especially African Americans or those who exercise regularly-can have CK levels 50-100% higher than average and still be perfectly fine. Here’s how to interpret results after starting a statin:- CK under 3x ULN and no symptoms? Keep taking the statin. No action needed.
- CK 3-10x ULN with muscle pain? Pause the statin, check thyroid and kidney function, and see a specialist. Don’t quit cold turkey.
- CK over 10x ULN? Stop the statin immediately. This is a red flag for rhabdomyolysis.
Why Do Some Guidelines Say Skip It?
The European Society of Cardiology calls baseline CK testing “optional.” Why? Because large studies, like the 2016 Cochrane Review of nearly 48,000 patients, found no difference in muscle injury rates between people who got tested and those who didn’t. And there’s another problem: false alarms. About 25-30% of healthy people have CK levels above the lab’s “normal” range-not because they’re sick, but because they lifted weights last week, got a flu shot in the arm, or had a long hike. If your doctor sees a high CK and assumes it’s the statin, you might get taken off a drug that’s saving your life. Dr. John Kastelein, a top European cardiologist, argues that baseline CK creates unnecessary anxiety and costs money without improving outcomes. In Canada, routine testing was estimated to cost $14.7 million a year with almost no impact on care. But here’s the flip side: when patients report muscle pain, having a baseline CK helps doctors avoid the “statin blame game.” In one study, practices that routinely checked baseline CK had 22% fewer unnecessary statin discontinuations. That’s huge-because stopping a statin in someone with heart disease can raise their risk of heart attack or stroke.
When Timing Matters
It’s not just whether you test-it’s when. If you get your CK drawn the day after a heavy workout, your levels will be sky-high. That’s not statin-related. That’s just muscle fatigue. So guidelines recommend testing within 4 weeks before starting the statin, but ideally within 2 weeks-and with clear instructions: no intense exercise for 48 hours before the test. Also, if you’ve had an intramuscular injection (like a steroid shot or vaccine) in the past week, that can spike CK too. Your doctor should ask about this. Documenting your activity level before the test isn’t just good practice-it’s critical for accurate interpretation.What About Genetic Testing?
There’s a new player: genetic testing for the SLCO1B1 gene variant. About 12% of Europeans carry this variant, which makes them 4.5 times more likely to develop muscle problems with simvastatin. If you know you have it, your doctor might choose a different statin or lower dose. But genetic testing isn’t widely available or covered by insurance yet. And it doesn’t help with other statins like atorvastatin or rosuvastatin as clearly. So for now, baseline CK is still the most practical tool for most people.Real-World Impact: Saving Money and Preventing Harm
Stopping a statin unnecessarily isn’t just risky-it’s expensive. For someone on a statin for secondary prevention (after a heart attack), each avoided discontinuation saves an estimated $2,850 in healthcare costs. That’s from avoiding repeat hospital visits, extra tests, and emergency care. In Australia, where statins are widely prescribed, an estimated 15-20% of patients who stop their statin due to muscle pain are doing so based on misleading or unexplained symptoms. Baseline CK helps cut through the noise. And here’s a quiet win: when patients know their baseline CK is normal, and then later develop pain, they’re more likely to trust their doctor’s advice to keep taking the statin if the CK hasn’t spiked. That builds confidence-and adherence.
The Bottom Line: Don’t Test Everyone, But Don’t Skip It When It Counts
Baseline CK testing isn’t a one-size-fits-all requirement. It’s a targeted tool. For healthy, young, low-risk patients on low-dose statins? Probably not needed. But if you’re older, have kidney issues, take other meds, or have a history of muscle pain with statins? Get the test. Get it right-no heavy exercise, no recent shots, and make sure your doctor records the exact number, not just “normal.” Statin therapy saves lives. But it’s not risk-free. Baseline CK doesn’t prevent muscle damage. But it gives you the data to make smarter decisions-when pain strikes, when levels climb, and when to keep going versus when to pause. The goal isn’t to avoid all side effects. It’s to avoid stopping a life-saving drug because of a false alarm.What If Your CK Is High Before You Even Start?
If your baseline CK is elevated and you don’t know why, don’t panic. But do pause. Your doctor should check for:- Hypothyroidism (a simple TSH test)
- Chronic kidney disease (eGFR)
- Recent trauma or intense exercise
- Neuromuscular disorders like muscular dystrophy or ALS
- Supplements like creatine or red yeast rice

Ross Ruprecht
November 23, 2025 AT 09:52Why are we even doing this test? I got my statin script and didn't even know CK was a thing until my pharmacist mentioned it. Felt like a scam.
Jennifer Skolney
November 24, 2025 AT 01:02I started statins last year and had muscle pain right away. My doctor wanted to pull me off until I showed him my baseline CK was normal. Turned out I just strained my back lifting boxes. Saved my heart and my sanity.
Charmaine Barcelon
November 24, 2025 AT 01:17People are so lazy now. If you're over 60 and on a statin, you should just get tested every time. No excuses. You're lucky you even have a heart to save.
Manjistha Roy
November 25, 2025 AT 19:47As someone who grew up in a household where medicine was always questioned, I appreciate how this breaks down the real science behind CK testing. It's not about fear-it's about knowing your body's baseline. This is the kind of clarity we need in public health communication.
Henrik Stacke
November 26, 2025 AT 16:54Having worked in primary care in the NHS for over a decade, I can confirm that baseline CK testing, when applied selectively, reduces unnecessary statin discontinuations by a significant margin. The real cost is not the test-it’s the cardiac events we prevent by keeping patients on therapy.
Demi-Louise Brown
November 26, 2025 AT 21:58My mom is 79 and has mild kidney disease. She was terrified of statins until her doctor ordered the baseline CK. It came back high-but it was from her daily walks. She kept the statin, and her LDL dropped 40%. This isn’t bureaucracy. It’s common sense.
Karla Morales
November 27, 2025 AT 08:56Let’s be real: 25-30% of people have elevated CK for no reason. That’s not a flaw in the test-it’s a flaw in the interpretation. Labs need to update their reference ranges. And doctors need to stop blaming statins for everything. 😒
Bryson Carroll
November 29, 2025 AT 04:12Oh wow another medical article pretending to be science. Baseline CK testing is a cash grab by labs and overworked PCPs who don’t want to think. The Cochrane review says it does nothing. End of story. Stop wasting people’s time.
JD Mette
November 30, 2025 AT 12:51I had a friend who got taken off statins after a high CK reading. Turned out he’d done 50 burpees the day before. He’s now had two heart attacks. I wish someone had told him to check his baseline first.
Kane Ren
December 2, 2025 AT 07:35My doctor didn’t even mention CK when I started atorvastatin. I asked. He said, ‘You’re young, healthy, and on a low dose-no need.’ Two months later I had cramps. Got tested. CK was 3x normal. We paused the drug, found a vitamin D deficiency, and I’m back on a lower dose now. Asking questions saved me.
Kezia Katherine Lewis
December 2, 2025 AT 22:21The SLCO1B1 genetic variant is underutilized but critical in populations with high statin intolerance. While baseline CK remains the pragmatic first step, we are entering an era where pharmacogenomics will redefine personalized lipid therapy. The infrastructure is lagging, but the science is unequivocal.