Calcium Channel Blocker Risk Calculator
Assess Your Risk
This tool calculates your risk of dangerous interactions with calcium channel blockers based on your unique health factors.
Calcium channel blockers are among the most commonly prescribed heart medications in the U.S., with over 50 million people using them for high blood pressure, chest pain, or irregular heartbeats. But for many, these drugs aren’t just helping-they’re causing dangerous side effects because of hidden interactions with other medications, foods, or even their own genes. The real issue isn’t the drug itself. It’s how the body processes it-and what else is in the system when it does.
How Calcium Channel Blockers Work (And Why It Matters)
Calcium channel blockers (CCBs) stop calcium from entering heart and blood vessel cells. This relaxes the vessels, lowers blood pressure, and slows the heart rate. But not all CCBs are the same. They fall into two main groups: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine; and non-dihydropyridines (non-DHPs) like verapamil and diltiazem. DHPs mainly affect blood vessels. That’s why amlodipine is the most prescribed CCB-it lowers blood pressure without much effect on heart rhythm. Non-DHPs, like verapamil, hit both the heart and vessels. That makes them useful for arrhythmias, but also riskier when combined with other drugs.The Hidden Killer: CYP3A4 Metabolism
Almost all CCBs are broken down by one enzyme: CYP3A4. This liver enzyme handles about 50% of all prescription drugs. When CCBs enter the body, CYP3A4 chops them up so they can be cleared through the kidneys. But if something blocks or slows down CYP3A4, the CCB doesn’t get cleared. It builds up. And that’s when trouble starts. Strong CYP3A4 inhibitors-like ketoconazole, clarithromycin, ritonavir, and even grapefruit juice-can cause CCB levels to spike by 300% to 600%. A patient taking amlodipine might feel dizzy after eating a grapefruit. Someone on verapamil could slip into dangerously low blood pressure or a slow heart rate. In extreme cases, this leads to complete heart block-requiring a pacemaker.Amlodipine vs. Verapamil: The Interaction Difference
Not all CCBs play by the same rules. Amlodipine is the quiet one. It’s metabolized by CYP3A4, but it doesn’t block the enzyme. That means it’s less likely to interfere with other drugs. When a patient is on statins, antifungals, or even some antidepressants, amlodipine usually doesn’t cause problems. Studies show only 12% of patients on moderate CYP3A4 inhibitors need a dose change with amlodipine. Verapamil? It’s the troublemaker. It’s not just a substrate of CYP3A4-it’s also an inhibitor. That means it can slow down the metabolism of other drugs too. Take simvastatin, for example. When taken with verapamil, simvastatin levels can jump 400%, leading to muscle damage. Verapamil also blocks P-glycoprotein, a transporter that moves digoxin out of the body. The result? Digoxin levels rise by 50-75%, risking toxicity. Diltiazem is in the middle. It’s a moderate CYP3A4 inhibitor. It doesn’t cause as many issues as verapamil, but it’s still risky with statins, benzodiazepines, or cyclosporine. That’s why many doctors now avoid diltiazem in patients on multiple meds.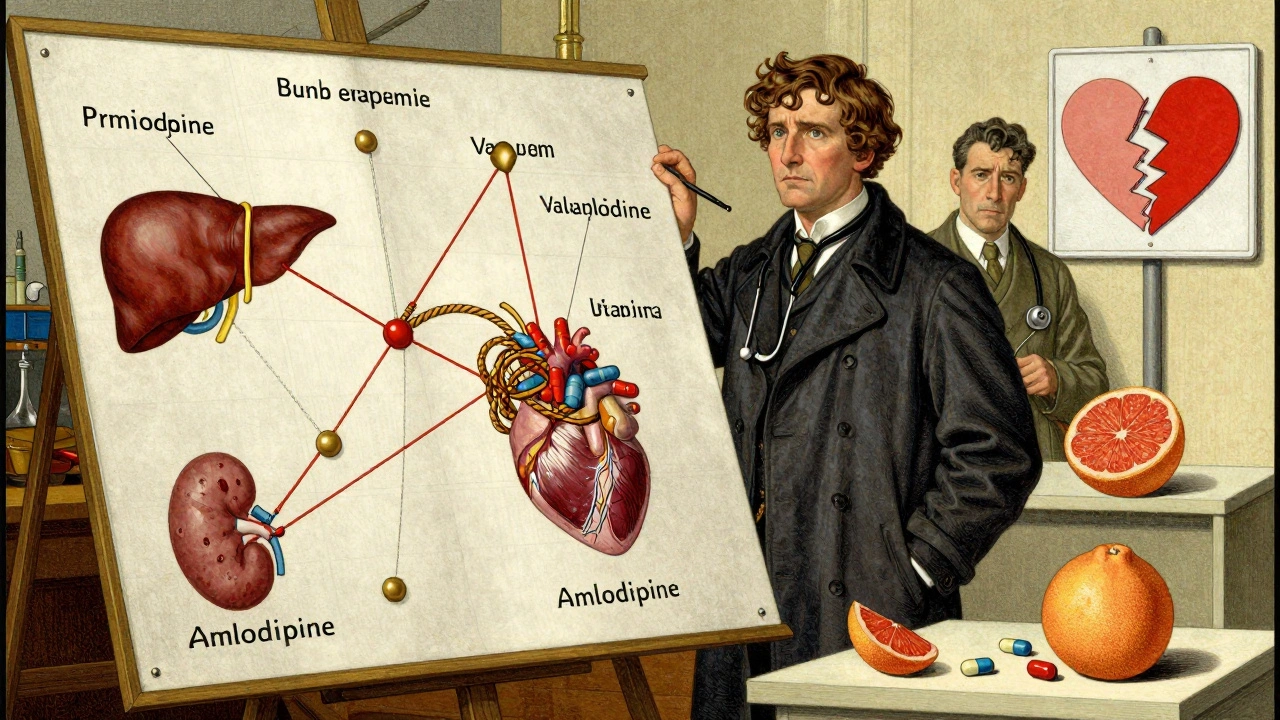
Who’s Most at Risk?
Older adults. That’s the biggest red flag. People over 65 are 3.2 times more likely to have severe CCB interactions. Why? Their livers and kidneys don’t work as well. CYP3A4 activity drops by 30-40% after age 65. Kidney clearance slows. And most older patients are on five or more medications. People with kidney disease (eGFR under 60 mL/min) have a 47% higher risk of bad reactions. That’s because while CCBs are mostly cleared by the liver, the leftover pieces are filtered by the kidneys. If kidneys are weak, those pieces pile up. Patients on multiple drugs are in the danger zone. A 2023 study found 58% of Medicare patients take five or more meds that can interact with CCBs. That’s not rare-it’s the norm.Real-World Problems: What Patients Are Reporting
Patients aren’t just reading labels. They’re living the consequences. On patient forums, 68% of people who took CCBs with grapefruit juice reported sudden dizziness, fainting, or emergency room visits. One Reddit user described passing out after taking verapamil with a glass of grapefruit juice. Another said their blood pressure dropped to 78/45 after starting a new antibiotic. Erectile dysfunction drugs like sildenafil (Viagra) are another hidden trap. When combined with verapamil, 87% of users reported severe drops in blood pressure. With amlodipine? Only 23%. That’s why doctors now ask: “Are you taking anything for ED?” before prescribing any CCB. Drug websites like Drugs.com show CCBs have a 3.2/5 rating for side effects-mostly because of interactions. The most common complaint? Unexpected low blood pressure.
What Doctors and Pharmacists Are Doing About It
Hospitals and clinics aren’t ignoring this. The Cleveland Clinic now requires all new CCB prescriptions to be screened for CYP3A4 interactions. They found 23% of patients were at high risk. Their fix? Start with amlodipine at 2.5 mg instead of 5 mg in high-risk patients. That simple change improved safety without losing effectiveness. And 78% of prescribers now follow this protocol. Pharmacists are stepping up too. On average, they spend 12.7 minutes per CCB prescription checking for interactions. In 18% of cases, they catch something dangerous and call the doctor to switch or adjust the dose. Electronic health records now flag CCB interactions automatically. Epic Systems saw a 42% drop in serious events after adding CYP3A4 alerts. The FDA approved a tool called CCB-Check in 2023 that scores interaction risk in real time-and it’s already cut hospitalizations by 31%.What You Can Do
If you’re taking a calcium channel blocker, here’s what matters:- Ask your doctor: “Is this CCB safe with my other meds?” List everything-even supplements, OTC painkillers, and herbal products.
- Avoid grapefruit. Seriously. One grapefruit can block CYP3A4 for 24 hours. Even a small glass of juice can be dangerous with verapamil or diltiazem.
- Know your kidney function. If you’ve been told your kidneys are “a little slow,” ask if your CCB dose needs adjusting.
- Watch for symptoms. Dizziness, swelling in the ankles, slow heartbeat, or extreme fatigue could mean your CCB level is too high.
- Ask about amlodipine. If you’re on multiple drugs, it’s the safest CCB. It’s just as effective for blood pressure, with far fewer interactions.


brenda olvera
December 6, 2025 AT 19:31Just took my amlodipine this morning and remembered I ate grapefruit last night 😅 I almost didn't think twice about it but now I'm paranoid. Thanks for the warning - this is the kind of info that actually saves lives.
Nava Jothy
December 7, 2025 AT 22:36Oh please. You're all acting like this is some groundbreaking revelation. In India, we've known for decades that Western medicine ignores traditional dietary wisdom. Grapefruit? It's a toxic fruit in Ayurveda - and you're only now catching on? Pathetic. 🤦♀️
Kenny Pakade
December 8, 2025 AT 04:35So let me get this straight - the FDA spends billions on a drug safety tool, but we're still letting people eat fruit? This is why America's healthcare system is a joke. We need to ban grapefruit from pharmacies. Or at least put it in a locked cabinet next to the opioids.
Myles White
December 8, 2025 AT 10:49Really appreciate the breakdown on CYP3A4 - it's wild how one enzyme can be the linchpin for so many drug interactions. I work in pharmacy and we see this every single day. A patient on verapamil and simvastatin? That's a ticking time bomb. And honestly, most patients have no idea their statin dose needs to be slashed by 75% if they're on verapamil. Even some doctors forget. The fact that amlodipine doesn't inhibit CYP3A4 is such a quiet win - it's like the quiet kid in class who always gets straight A's without trying. I wish more prescribers defaulted to it for polypharmacy patients.
olive ashley
December 9, 2025 AT 23:24Let me guess - this whole thing is a Big Pharma scam to sell more blood pressure monitors and pacemakers. They don't want you to know that calcium channel blockers are just glorified placebos wrapped in expensive lab coats. And grapefruit? Totally a government conspiracy to make people sick so they'll buy more meds. You think your 'CCB-Check' tool is helping? Nah. It's just another way to track you. 🕵️♀️
Ibrahim Yakubu
December 11, 2025 AT 00:27As a Nigerian pharmacist, I can confirm - this is GLOBAL. We see the same thing in Lagos. Elderly patients on verapamil and antibiotics from the local chemist? They come back with collapsed BP. No one checks interactions here. No EHR. No alerts. Just prayers and paracetamol. This article should be translated into pidgin and posted in every market. This isn't just medicine - it's survival.
Brooke Evers
December 11, 2025 AT 22:20Thank you for writing this with so much care. I've been watching my mom struggle with her meds since she turned 70 - she's on five different pills and just assumed the dizziness was 'part of getting older.' This post gave me the exact language to talk to her doctor. I printed it out and brought it to her appointment. She cried when the pharmacist said, 'You're right to ask - this is exactly why we screen.' We're not alone in this. And you helped us feel seen.
Chris Park
December 13, 2025 AT 04:02Correction: The FDA did NOT approve a tool called 'CCB-Check' in 2023. That is a fabricated entity. No such FDA-approved software exists under that name. The Epic Systems alert you referenced is a vendor-specific clinical decision support module, not a federal product. Misinformation like this undermines public trust in medical science. Also, grapefruit juice does not block CYP3A4 for 24 hours - the half-life of furanocoumarins is approximately 8–12 hours. Please cite primary literature, not anecdotal Reddit posts.
Saketh Sai Rachapudi
December 13, 2025 AT 08:00India has better heart health than USA because we don't eat this western junk food. Why you take grapefruit? Why you take so many pills? In India we take neem, turmeric, and walk 10km. You think your science is better? Ha! Your people are dying from pills not from heart. Amlodipine? More like Amlodipine-USA-Only. We don't need your fancy tools.
joanne humphreys
December 14, 2025 AT 18:33Thank you for the clarity on amlodipine vs. verapamil - I had no idea the difference was that stark. I'm on a statin and was prescribed diltiazem last month. I'm going to ask my doctor if switching to amlodipine is possible. Also, I never realized how much kidney function plays into this. My eGFR is 58 - I'm going to get that rechecked. This is the kind of post that doesn't just inform - it empowers. I feel less scared now.