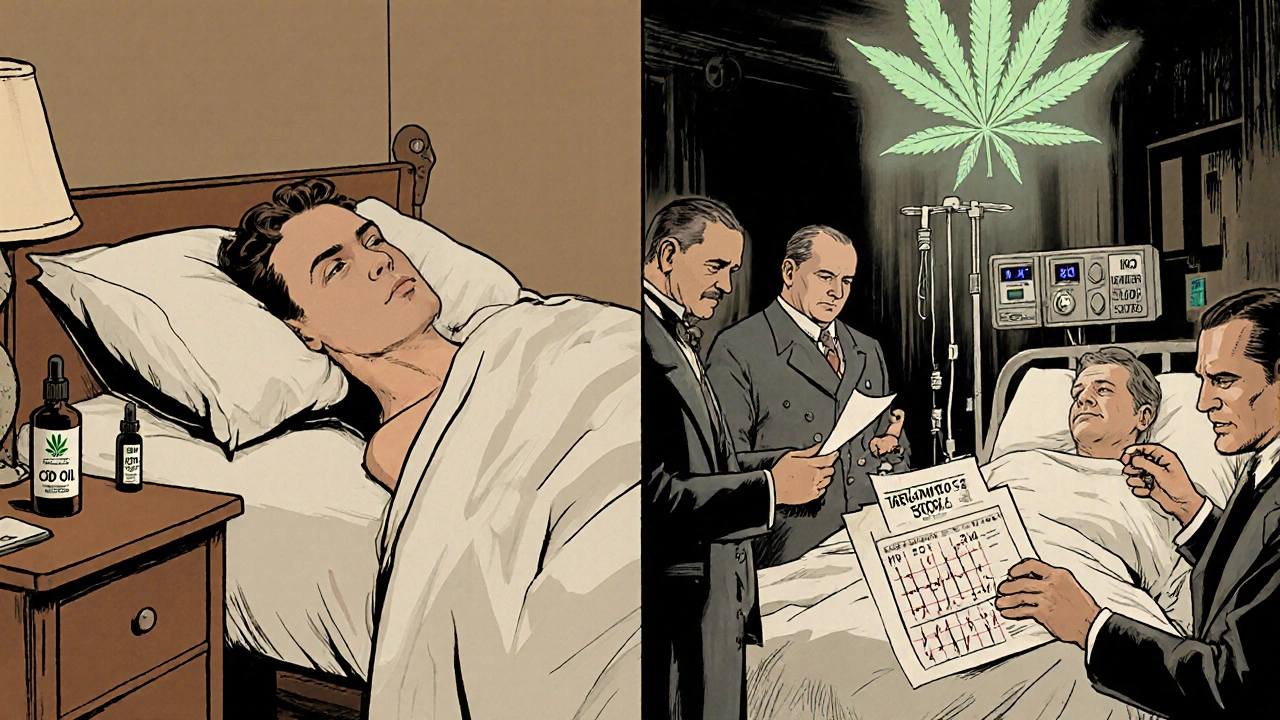
More people are using cannabis - whether it’s CBD oil for anxiety, THC for chronic pain, or full-spectrum products for sleep - and many are taking prescription drugs at the same time. But here’s the problem: cannabis doesn’t just sit quietly in your body. It actively interferes with how your medications work, sometimes in ways that can be dangerous or even life-threatening.
How Cannabis Changes How Your Medications Work
Cannabis doesn’t interact with medications the same way alcohol or grapefruit juice does. Its effects are deeper, more complex, and often hidden. The main culprit? Enzymes in your liver - specifically, the cytochrome P450 family. These enzymes break down about 60% of all prescription drugs. CBD and THC block them. When that happens, your medications don’t get processed the way they should.
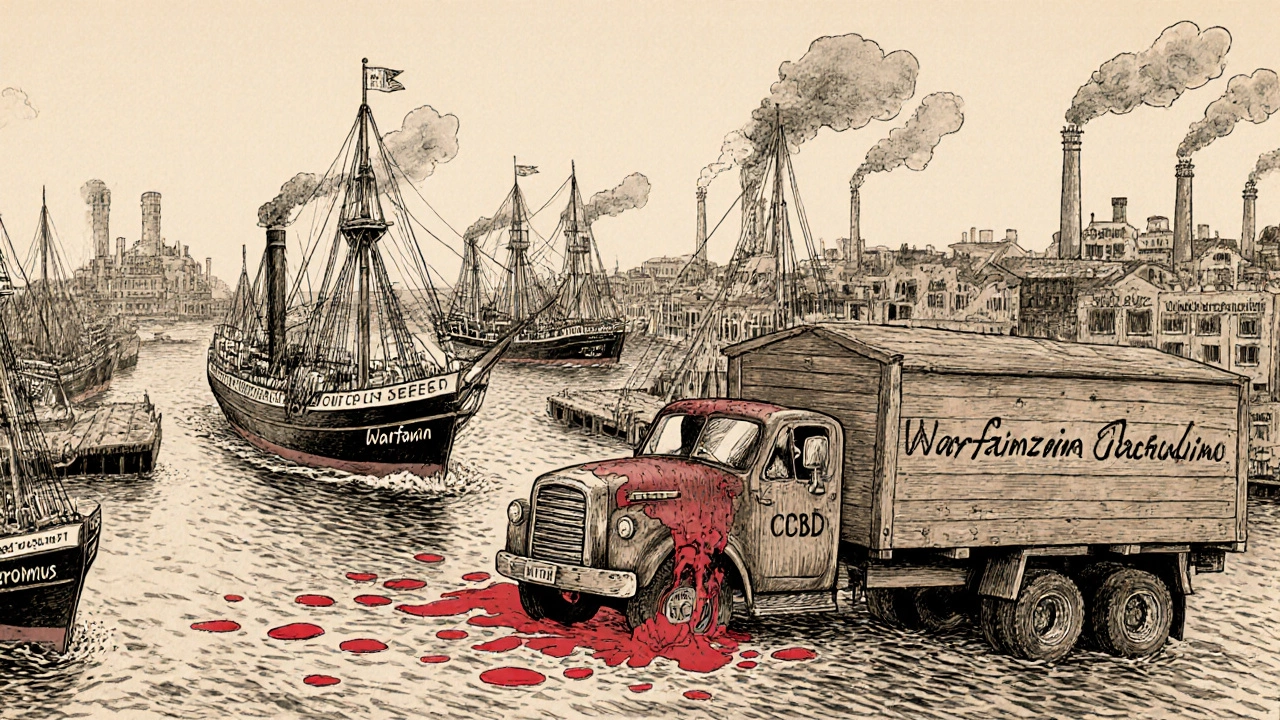
Think of it like traffic. Your liver is a busy intersection. Medications are cars trying to get through. Normally, enzymes are the traffic lights that let them pass at the right time. But when you add CBD or THC, it’s like putting a big truck in the middle of the road - everything slows down or backs up. That means drugs like warfarin, clobazam, or tacrolimus build up in your blood, increasing the risk of overdose or side effects.
Even small doses matter. A 2023 study found that CBD doses as low as 5-10 mg per day can start affecting how your body handles certain drugs. At 20 mg or more, the risk jumps significantly. And it’s not just about the amount - the type of product matters too. Full-spectrum CBD (which includes trace THC) is 22-37% more likely to interfere with liver enzymes than pure CBD isolate. That’s because THC and other cannabinoids work together in what’s called the “entourage effect.”
High-Risk Interactions: When Cannabis Can Be Dangerous
Some medications are extremely sensitive to cannabis. Mixing them can lead to serious harm. Here are the biggest red flags:
- Warfarin (Coumadin): This blood thinner has a narrow safety window. Too little, and you risk clots. Too much, and you bleed internally. Studies show that CBD can increase warfarin levels by 29-48% within 72 hours. That’s enough to push INR levels into dangerous territory - one study documented 12 cases of life-threatening bleeding in patients using both. The American Society of Health-System Pharmacists now recommends checking INR every 3-5 days if you’re using cannabis, not weekly.
- Tacrolimus and Cyclosporine: These are used after organ transplants to prevent rejection. Cannabis can spike tacrolimus levels by 300-500%. A single dose of CBD oil could mean your body rejects a new kidney or liver. Transplant centers now routinely ask patients about cannabis use.
- Clobazam: Used for epilepsy, especially in children with Dravet syndrome. CBD increases clobazam levels by 60-500%. In one case, a patient couldn’t walk straight after starting CBD. Their neurologist cut the clobazam dose by 40% immediately. This isn’t rare - 63% of CBD users on clobazam report increased drowsiness.
These aren’t theoretical risks. They’re documented in clinical reports, hospital records, and patient forums. Reddit’s r/MedicalCannabis has hundreds of posts from people who didn’t realize their CBD oil was making their meds too strong - until they ended up in the ER.
Moderate-Risk Interactions: Watch for Signs
These combinations won’t always cause disaster, but they can make things worse - and you might not notice until it’s too late.
- Benzodiazepines (alprazolam, diazepam): Both cannabis and these drugs slow down your central nervous system. Together, they can cause extreme drowsiness, confusion, and impaired coordination. In elderly patients, this increases fall risk by 47%. One user on Reddit said they passed out after taking CBD with Xanax - and had no memory of it.
- Opioids (oxycodone, morphine): Cannabis can reduce how quickly your body clears opioids, increasing the risk of respiratory depression. While some people use them together for pain, the effect isn’t predictable. One study found morphine clearance dropped by 20-30% with CBD use.
- Calcium channel blockers (amlodipine, diltiazem): These lower blood pressure. Cannabis can boost their levels by 30-40%, leading to dizziness, fainting, or dangerously low blood pressure. One patient reported passing out after starting CBD while on amlodipine.
Unlike the high-risk interactions, these effects can be subtle. You might just feel “more tired than usual” or notice your blood pressure monitor showing lower numbers. That’s why monitoring matters.

Lower-Risk Interactions - But Still Not Risk-Free
Some medications show minimal interaction with cannabis, but that doesn’t mean they’re safe.
- SSRIs (sertraline, fluoxetine): CBD may raise sertraline levels by 10-15%. But in most cases, this doesn’t cause noticeable side effects. A 2023 survey found 41% of users on SSRIs reported no change when adding CBD. Still, if you’re prone to serotonin syndrome or have a history of mood swings, proceed with caution.
- Statins (atorvastatin): CBD can increase atorvastatin levels by 20-25%. So far, no cases of rhabdomyolysis (muscle breakdown) have been linked to this combo - but the data is limited.
Here’s the catch: just because you haven’t had a problem doesn’t mean you won’t. Everyone’s liver works differently. Genetics, age, diet, and other medications all play a role. What’s safe for one person might be risky for another.
How You Take Cannabis Changes Everything
Not all cannabis use is the same. The way you take it affects how quickly and how long it interferes with your meds.
- Smoking or vaping: THC hits your bloodstream in 6-10 minutes. If you’re on a sedative or blood pressure med, the interaction can be sudden and intense - especially if you use it recreationally on weekends.
- Oral CBD (oils, gummies): Takes 2-4 hours to peak and lasts 6-8 hours. This creates a longer window for interaction. Warfarin users who take CBD in the morning might not see INR changes until the next day.
- Cannabis tea or edibles: Effects are slower and more unpredictable. Some studies show tea doesn’t affect certain chemo drugs like docetaxel - but others show it can lower theophylline levels by 25-30% due to enzyme induction.
There’s no universal rule. One person might smoke cannabis daily with no issues on their blood pressure meds. Another might get dizzy after one gummy. That’s why personalized care matters.
What You Should Do - Step by Step
If you’re using cannabis and take any prescription drugs, here’s what to do:
- Be honest with your doctor and pharmacist. Don’t say “I take CBD sometimes.” Say: “I take 25 mg of full-spectrum CBD oil every night for sleep.” Include frequency, dose, and product type.
- Check your meds. Use tools like the University of Washington’s Cannabis Drug Interactions database (updated quarterly). Look up your specific drugs - especially if they’re blood thinners, seizure meds, or transplant drugs.
- Get baseline tests. If you’re on warfarin, tacrolimus, or clobazam, ask for a blood test before starting cannabis. This gives you a reference point.
- Monitor closely after starting. For warfarin: check INR 48-72 hours after your first dose of CBD. For clobazam: watch for drowsiness, confusion, or trouble walking. For blood pressure meds: track your readings daily for the first week.
- Adjust slowly. If your doctor recommends lowering your medication dose, reduce it by 10-25% at first. Don’t make big cuts without guidance.
Pharmacists in Pennsylvania are now required to warn patients: “Even weekend cannabis use can triple your bleeding risk if you’re on warfarin.” That’s not an exaggeration. It’s based on real cases.
What’s Missing - And Why It Matters
Here’s the scary part: we don’t know enough. Most studies focus on epilepsy or cancer patients. What about people with diabetes, heart disease, or depression? Only 12 studies have looked at cannabis and diabetes meds - even though 28% of cannabis users have diabetes. We don’t know how it affects GLP-1 agonists like Ozempic. We don’t know how long-term use affects liver health. We don’t know how it interacts with newer antidepressants or antivirals.
And the products are changing fast. A 2023 survey found that 76% of community pharmacists feel unprepared to answer questions about cannabis interactions - even though 68% see patients with these issues every month. Most CBD products aren’t regulated. A bottle labeled “10 mg CBD” might actually have 18 mg - or hidden THC. That’s why dosing is so unpredictable.
Bottom Line: Don’t Assume It’s Safe
Cannabis isn’t a magic bullet. And it’s not harmless when mixed with medications. Some people use it safely with their prescriptions. Others end up in the hospital. The difference? Awareness.
If you’re on any medication - especially blood thinners, seizure drugs, or transplant meds - don’t start CBD or THC without talking to your doctor. Don’t rely on Reddit advice or YouTube videos. Don’t assume “natural” means “safe.”
The science is clear: cannabis changes how your body handles drugs. It’s not a guess. It’s chemistry. And chemistry doesn’t care if you think it’s harmless. It just works.
Ask your doctor: “Could my cannabis use be affecting my meds?” If they don’t know, ask for a referral to a pharmacist who specializes in drug interactions. That’s the safest path forward.
Can I take CBD with my blood thinner like warfarin?
No - not without close medical supervision. CBD can increase warfarin levels by up to 48%, raising your INR and risk of dangerous bleeding. Studies show 12 cases of life-threatening bleeding in patients using both. If you must use CBD, your doctor will need to check your INR every 3-5 days instead of weekly, and may lower your warfarin dose by 10-25%.
Does THC interact with medications the same way as CBD?
Not exactly. CBD is a stronger inhibitor of CYP3A4 and CYP2C19, while THC mainly affects CYP1A2 and CYP2C9. Both can interfere with warfarin, but THC may be more likely to reduce the effectiveness of HIV medications like protease inhibitors by 30-40%. Full-spectrum products (with both THC and CBD) are more likely to cause interactions than CBD isolate.
Is it safe to use CBD with antidepressants like sertraline?
Most people don’t notice problems, but there’s a small risk. CBD can raise sertraline levels by 10-15%, which might increase side effects like nausea or jitteriness - especially at higher doses. If you’re sensitive to SSRIs or have a history of serotonin syndrome, start with a low CBD dose and watch for changes in mood or energy. Always tell your doctor.
Can I take CBD with my pain meds like oxycodone?
It’s possible, but risky. CBD can slow how quickly your body clears oxycodone, increasing the chance of drowsiness, slowed breathing, or overdose. Some users report no issues, but others have needed emergency care. If you use both, avoid driving, monitor for excessive sleepiness, and never increase your dose without talking to your doctor.
How long should I wait between taking CBD and my other medications?
Some sources suggest waiting 2 hours, but there’s little evidence this works. CBD and THC affect liver enzymes for hours - sometimes days. Spacing them out won’t prevent the interaction. The only reliable way to avoid problems is to monitor your blood levels (like INR or drug concentrations) and adjust doses under medical supervision.
Are over-the-counter CBD products safe to use with prescriptions?
No - and here’s why: most aren’t regulated. A 2022 FDA study found 70% of CBD products didn’t contain the amount listed on the label. Some had hidden THC, contaminants, or much higher CBD than advertised. If you’re on a medication with a narrow safety window, you can’t risk guessing. Only use products tested by a third party and prescribed by a doctor.
What should I do if I’ve already been using cannabis with my meds?
Don’t stop suddenly - that can be dangerous. Tell your doctor what you’ve been using, how much, and how often. Ask for a blood test to check your medication levels. If you’re on warfarin, get an INR test. If you’re on clobazam or tacrolimus, ask for a drug level check. Then work with your provider to adjust doses safely.

Jennifer Stephenson
November 16, 2025 AT 16:54Just stopped my CBD oil after reading this. My INR was creeping up last week. Thanks for the clarity.
Philip Rindom
November 17, 2025 AT 20:02Wow. So the guy who sold me that ‘10mg CBD’ gummy off Instagram was lying? And I thought I was being smart by avoiding pills. 🤦♂️
Eric Gregorich
November 18, 2025 AT 01:20Let’s be real - this isn’t about science. It’s about control. The pharmaceutical industry hates that people are finding relief without their $500/month pills. They’re scared. So they turn ‘possible interaction’ into ‘life-threatening danger’ to scare folks back into their cages. I’ve been on warfarin for 8 years and CBD for 3. My INR? Stable. My quality of life? Infinite. Don’t let fear dictate your healing. 🌿
Laura-Jade Vaughan
November 19, 2025 AT 03:25OMG I’m literally crying 😭 I just realized my ‘natural’ CBD gummies were probably why I passed out at yoga last week. I was on Xanax AND CBD. I thought I was just ‘relaxed.’ Turns out I was basically drunk with a side of existential dread. 🙈 Thank you for this. I’m getting my INR checked tomorrow. Also, full-spectrum is a trap. I’m switching to isolate. And no, I don’t care if it’s ‘less effective.’ I’d rather live.
Koltin Hammer
November 19, 2025 AT 16:08This is why I love the global perspective. In India, we’ve used cannabis in Ayurveda for centuries - but always with context, ritual, and a guru who knew your dosha. Here? We treat it like a vitamin. Pop a gummy, scroll TikTok, and call it self-care. We’ve lost the wisdom. The science is real, yes - but the culture around it is broken. We need both: the biochemistry AND the mindfulness. Otherwise, we’re just trading one addiction for another. 🙏
Connor Moizer
November 20, 2025 AT 08:18Bro, if you’re on tacrolimus and think a ‘little CBD’ won’t kill your transplant, you’re not just reckless - you’re a liability to the whole system. I work in a transplant unit. Saw a guy lose his liver because he ‘didn’t think it mattered.’ He was 24. Don’t be that guy. Get tested. Talk to your pharmacist. Or don’t. But don’t act surprised when you’re on a ventilator.
Erika Lukacs
November 21, 2025 AT 09:48It’s fascinating how we’ve pathologized natural substances while glorifying synthetic ones. The liver doesn’t care if it’s CBD or fluoxetine - it just wants to metabolize. But we’ve built a system that profits from confusion. The real issue isn’t cannabis - it’s the lack of regulation, education, and trust in patient autonomy.
Parv Trivedi
November 21, 2025 AT 10:38As someone from India, I’ve seen my uncle take ashwagandha with blood pressure meds - no issues. But he never mixed it with THC. The key is balance, not fear. If you’re careful, informed, and monitor, you can use cannabis safely. But ignorance? That’s the real danger. Talk to your doctor. Not Reddit. Not your cousin who ‘swears by it.’
Victoria Short
November 23, 2025 AT 04:52So… I’m just supposed to stop feeling better? Cool. I’ll just go back to feeling like a zombie on SSRIs. Thanks for the guilt trip.
Rebekah Kryger
November 24, 2025 AT 08:22Y’all are acting like CBD is a new drug. It’s a plant. Plants have been interacting with pharmaceuticals since we invented pills. The real problem? The FDA doesn’t regulate it. So of course people get screwed. But blaming the plant? That’s like blaming a hammer because someone used it to break a window. Fix the system. Not the herb.
Phil Best
November 25, 2025 AT 07:20I’m a veteran. I take 40mg of CBD nightly for PTSD. I’m also on lisinopril and sertraline. My VA doc didn’t blink. He said, ‘Track your BP and mood. Come back in two weeks.’ We did. Everything held. So yeah - it’s not magic. It’s medicine. And if your doctor doesn’t get it? Find one who does. Don’t let ignorance be your barrier.
Willie Randle
November 27, 2025 AT 04:44Let’s clarify terminology: ‘CBD isolate’ is pure cannabidiol. ‘Full-spectrum’ contains terpenes, flavonoids, and trace THC (<0.3%). The entourage effect is real - but so is the enzyme inhibition. The data is clear: full-spectrum increases interaction risk by 22–37%. That’s not a nuance. It’s a statistical fact. If you’re on warfarin, tacrolimus, or clobazam - choose isolate. Or abstain. There’s no middle ground that’s safe without monitoring.
kanishetti anusha
November 29, 2025 AT 03:09I’ve been using CBD for anxiety since my son was born. I’m on levothyroxine. I started with 5mg, checked my TSH after 2 weeks - still perfect. I slowly increased to 15mg. Still fine. But I didn’t just ‘start.’ I observed. I tracked. I talked to my endocrinologist. This isn’t about fear. It’s about responsibility. You can do both: heal and be safe.
Segun Kareem
November 30, 2025 AT 12:59Every time we label something ‘dangerous’ without understanding its context, we lose a piece of our humanity. Cannabis isn’t the enemy. Fear is. The system that silences conversation is the enemy. The pharmacy that sells untested oil is the enemy. The doctor who refuses to learn is the enemy. Not the plant. Not the person trying to feel better. We need more compassion, not more warnings. Let people choose - with knowledge, not panic.
roy bradfield
December 2, 2025 AT 06:26THIS IS A GOVERNMENT PLOY. The FDA, Big Pharma, and the DEA are all connected. They don’t want you to know that hemp oil can replace 80% of your prescriptions. That’s why they flooded the market with unregulated CBD - so they can scare you with fake studies and then sell you ‘FDA-approved’ synthetic versions at $1,200 a bottle. The war on cannabis isn’t about safety - it’s about profit. Wake up. The truth is in the liver enzymes - and they’re being manipulated by the same people who gave you opioids.