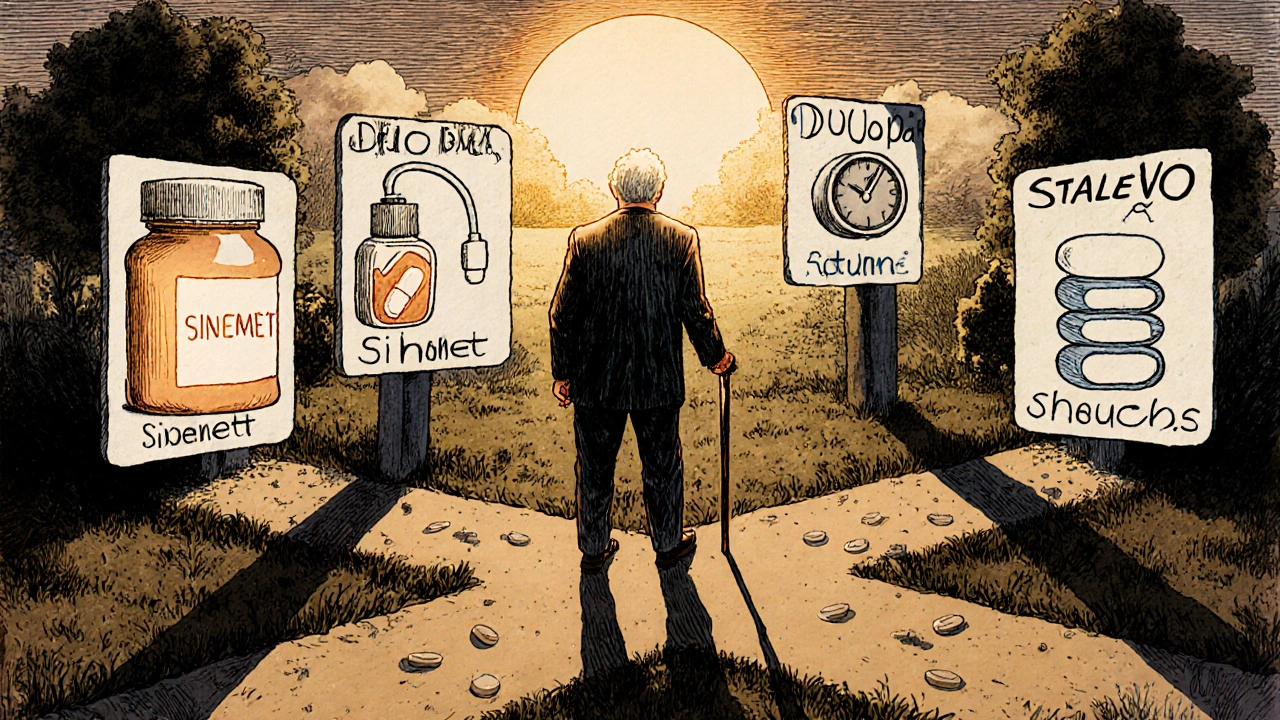
When you’re managing Parkinson’s disease, finding the right medication isn’t just about symptom control-it’s about daily life. Sinemet, a combination of carbidopa and levodopa, has been the gold standard for decades. But it’s not the only option anymore. Many people on Sinemet start noticing its limits: the wearing-off periods, the nausea, the unpredictable movements. That’s when they ask: Sinemet-is there something better?
What Sinemet Actually Does
Sinemet combines two drugs: levodopa, which your brain turns into dopamine, and carbidopa, which stops levodopa from breaking down too early in your body. Without carbidopa, up to 95% of levodopa would be wasted before it ever reaches the brain. With it, you get more dopamine where it’s needed-and fewer side effects like vomiting.
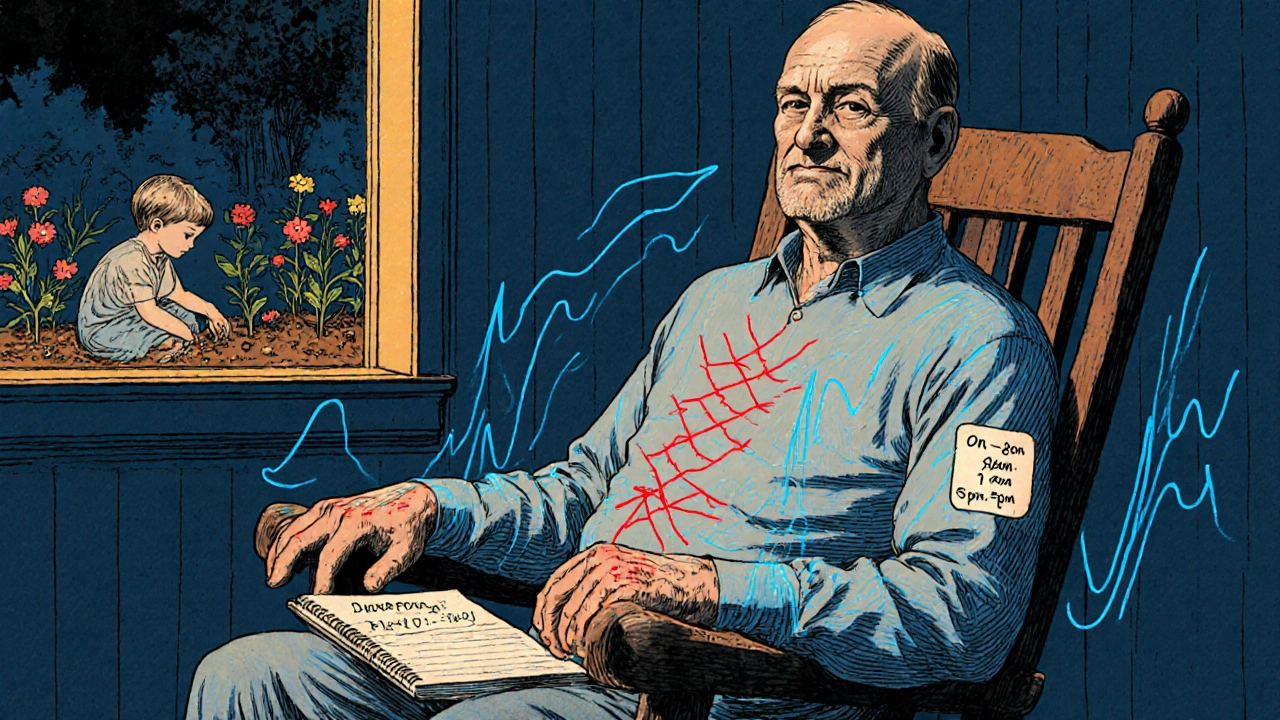
But here’s the catch: levodopa doesn’t last forever. Over time, as Parkinson’s progresses, the brain’s ability to store and release dopamine fades. That’s why people on Sinemet often start feeling the effects wear off after just 2-3 hours. The medication stops working before the next dose kicks in. This leads to the dreaded ‘on-off’ cycles: one moment you’re moving freely, the next you’re frozen.
Why People Look for Alternatives
It’s not just about effectiveness. Sinemet comes with a long list of side effects: dizziness, low blood pressure, hallucinations, and sudden sleep attacks. Some people can’t tolerate the nausea. Others hate the fact they have to take it 3-4 times a day on an empty stomach. And for those with advanced Parkinson’s, swallowing pills becomes harder.
That’s why alternatives aren’t just nice to have-they’re necessary for many. The goal isn’t to ditch Sinemet entirely, but to find options that offer smoother symptom control, fewer side effects, or simpler dosing.
Duopa: The Levodopa Pump
If you’ve been on Sinemet for years and your symptoms are getting harder to manage, Duopa might be the next step. It’s not a pill-it’s a gel. Duopa delivers carbidopa and levodopa directly into your small intestine through a small tube connected to a portable pump.
The pump runs 16 hours a day, giving you a steady drip of medication instead of spikes and drops. This means fewer ‘off’ periods, less dyskinesia (involuntary movements), and more consistent mobility. Studies show people using Duopa spend up to 3.5 fewer hours per day in the ‘off’ state compared to oral Sinemet.
But it’s not simple. You need surgery to place the tube into your stomach (a PEG-J procedure). The pump has to be refilled daily. The tube can get clogged or infected. It’s a major commitment-but for people with advanced Parkinson’s who’ve run out of pill options, it’s life-changing.
Neupro Patch: Transdermal Rotigotine
Not everyone wants pills or pumps. The Neupro patch offers a patch-and-forget option. It delivers rotigotine, a dopamine agonist, through your skin once a day.
Unlike Sinemet, which replaces dopamine, Neupro mimics dopamine’s effect directly on brain receptors. That means it doesn’t rely on your brain to convert anything. It works steadily, day and night.
It’s especially helpful for early-stage Parkinson’s patients who want to delay starting levodopa, or for those who struggle with swallowing. It also helps with nighttime symptoms like restless legs.
Downsides? Skin irritation is common. The patch can fall off if you sweat a lot. And because it’s not levodopa, it doesn’t work as well for advanced cases. Some people report dizziness, sleepiness, or impulse control issues-like gambling or binge eating.

Stalevo: Sinemet Plus Entacapone
Stalevo is essentially Sinemet with an extra ingredient: entacapone. This drug blocks an enzyme that breaks down levodopa in the bloodstream. The result? More levodopa reaches the brain, and it lasts longer.
For people who still get good results from Sinemet but notice it wears off too quickly, Stalevo can extend the ‘on’ time by 1-2 hours per dose. It’s a simple switch-same pills, just one extra component.
But it’s not magic. Side effects are similar to Sinemet, just more likely: diarrhea, orange urine (harmless), and increased dyskinesia. You still have to take it multiple times a day. And it won’t help if your brain has lost too many dopamine-producing cells.
Parcopa: Fast-Dissolving Sinemet
Swallowing pills gets harder as Parkinson’s progresses. That’s where Parcopa comes in. It’s the same carbidopa-levodopa combo as Sinemet, but it dissolves on your tongue-no water needed.
It’s ideal for people who have trouble swallowing, who are nauseous, or who need quick relief during an ‘off’ episode. Because it absorbs faster, it can kick in 10-15 minutes quicker than regular Sinemet.
It’s not cheaper. It’s not stronger. But for those who’ve struggled with pills, it’s a game-changer. One user in Melbourne told me: ‘I used to carry a water bottle everywhere. Now I just pop a tablet in my mouth and go.’
Amantadine and Other Non-Levodopa Options
Not every alternative is a levodopa version. Amantadine, originally an antiviral, is now used to reduce dyskinesia caused by long-term levodopa use. It doesn’t replace dopamine-it helps smooth out the wild movements.
Other dopamine agonists like pramipexole (Mirapex) and ropinirole (Requip) are often used early in the disease. They’re less effective than levodopa for movement symptoms, but they have a lower risk of causing dyskinesia. Many doctors start patients on these to delay levodopa use.
But they come with their own risks: hallucinations, swelling in the legs, and sudden sleep episodes. One study found 1 in 5 people on pramipexole had compulsive behaviors like shopping or sex. That’s why they’re not a first choice for older adults or those with mental health history.
MAO-B Inhibitors: Rasagiline and Selegiline
These drugs don’t replace dopamine. They stop your brain from breaking it down. Rasagiline (Azilect) and selegiline (Eldepryl) are often used as add-ons to Sinemet, especially in early Parkinson’s.
They’re mild. You might notice slightly better movement or a small delay in symptom worsening. But they’re not powerful enough on their own for most people.
Selegiline can interact with certain antidepressants and foods high in tyramine (aged cheese, cured meats). Rasagiline is safer in that regard. Both can cause dizziness or insomnia. They’re not replacements for Sinemet-but they can help stretch its effect.
When to Consider Alternatives
There’s no rush to switch. Sinemet still works well for most people in the first 5-7 years. But here are signs it’s time to talk to your neurologist:
- You’re having more than two ‘off’ periods a day
- Your ‘on’ time lasts less than 2 hours after a dose
- You’re getting dyskinesia (involuntary jerking) even with low doses
- You can’t swallow pills reliably
- You’re experiencing hallucinations or sudden sleep attacks
Switching isn’t about failure. It’s about adapting. Parkinson’s changes. Your treatment should too.
What Doesn’t Work
Many people try herbal supplements, high-dose vitamin B6, or CBD oil thinking they’ll replace Sinemet. None of these have proven effectiveness in clinical trials. Some, like high-dose B6, can actually interfere with levodopa.
Don’t replace your medication with unproven options. But do talk to your doctor about complementary approaches: physical therapy, tai chi, or speech therapy. These won’t stop Parkinson’s-but they can help you move better, speak clearer, and stay independent longer.
Final Thoughts: It’s About Personal Fit
There’s no single best alternative to Sinemet. What works for one person might be useless-or dangerous-for another. Your age, how long you’ve had Parkinson’s, your other health conditions, and even your daily routine all matter.
Some people thrive on the Neupro patch. Others need the precision of Duopa. Some just need Parcopa to get through breakfast. Stalevo helps extend the life of Sinemet without major changes.
The key is to track your symptoms. Keep a simple log: when you take your meds, when you feel ‘on’ or ‘off,’ any side effects. Bring it to your neurologist. Don’t wait until things get bad.
Medication for Parkinson’s isn’t a one-time fix. It’s a conversation that evolves. And the best option is the one that lets you live your life-without being ruled by the clock or the tremors.
Can I switch from Sinemet to another medication on my own?
No. Never change your Parkinson’s medication without your neurologist’s guidance. Levodopa and its alternatives affect brain chemistry in complex ways. Stopping suddenly can cause dangerous withdrawal symptoms like fever, confusion, or muscle rigidity. Always work with your doctor to adjust your treatment plan safely.
Is Duopa better than Sinemet?
Duopa is more effective for advanced Parkinson’s patients who have severe ‘off’ periods despite taking Sinemet multiple times a day. It provides steady dopamine delivery, reducing fluctuations. But it’s not better for everyone. It requires surgery, daily pump maintenance, and carries infection risks. For early-stage patients, Sinemet remains simpler and safer.
Does Neupro patch work as well as Sinemet?
No. Neupro is a dopamine agonist, not levodopa. It’s less effective at controlling core Parkinson’s movement symptoms like slowness and stiffness. It’s often used in early stages or as an add-on-not as a direct replacement for Sinemet. It’s best for people who can’t tolerate levodopa or want to delay starting it.
Are there generic versions of Sinemet?
Yes. Generic carbidopa-levodopa is widely available and just as effective as brand-name Sinemet. The only difference is cost-generics are significantly cheaper. Parcopa and Stalevo don’t have generics yet, but generic Sinemet is a solid, affordable option for most people.
How do I know if I need a different medication?
Track your symptoms daily. If you’re spending more than 2 hours a day in an ‘off’ state, if your doses don’t last as long as they used to, or if side effects like nausea, dizziness, or hallucinations are getting worse, it’s time to talk to your doctor. These are signs your current treatment needs adjustment.

Diane Thompson
October 31, 2025 AT 10:17Ugh, Sinemet makes me so nauseous I can’t even eat breakfast. Just switched to Neupro patch and life’s 10x better-no pills, no vomit, just stick it on and forget it.
Helen Moravszky
November 2, 2025 AT 07:50OMG YES I JUST STARTED PARCOPA LAST WEEK AND IT’S A GAME CHANGER!! I used to carry water everywhere just to swallow my meds, now I just pop it on my tongue and go. No more panic attacks before breakfast 😭 thank you for this post!!
Reginald Matthews
November 3, 2025 AT 23:15I’ve been on Sinemet for 8 years and just last month my neurologist added Stalevo. It’s not a miracle, but my ‘off’ periods dropped from 4 hours a day to under 2. The orange urine freaked me out at first-thought I was bleeding-but turns out it’s totally normal. Worth it.
Still take it 4x a day, but the extra hour of mobility? Worth the hassle.
Debra Callaghan
November 4, 2025 AT 13:39Don’t fall for the hype. CBD oil and supplements are scams. I tried them all-lost money, lost time, lost hope. Sinemet works. If you can’t handle it, talk to your doctor, don’t go chasing TikTok cures.
Mitch Baumann
November 4, 2025 AT 22:50As a former clinical pharmacologist (Ph.D., Johns Hopkins), I must emphasize: Duopa is the *only* truly rational solution for advanced PD. The pharmacokinetic profile is *superior*-Cmax, Tmax, AUC… all optimized. 📈 The PEG-J procedure? Minor compared to the QoL gains. 🤖✨
Neupro? Cute. But dopamine agonists are *not* levodopa. You’re not replacing the neurotransmitter-you’re hijacking the receptor. Aesthetic, perhaps. Therapeutic? Debatable.
And please, for the love of dopamine receptors-stop calling Parcopa ‘magic.’ It’s just a faster-absorbing formulation. Nothing more. 😌
Gina Damiano
November 5, 2025 AT 14:41I just want to say-my husband started Duopa last year and he’s laughing again. He hasn’t laughed in years. I know it sounds dramatic, but I swear, the pump gave him back his dignity. Not the meds. Not the pills. The *steady* drip.
He still hates the tube. Still complains about refills. But he dances in the kitchen now. And that’s all that matters.
Emily Duke
November 6, 2025 AT 07:44Y’all are so obsessed with meds. Have you tried acupuncture? Or tai chi? Or even just… walking? My aunt’s PD got better with daily walks in the park-no drugs. Just sunlight and fresh air. You’re all too quick to pop pills.
And don’t even get me started on those ‘experts’ who say CBD works. Pfft. Big Pharma doesn’t want you to know the truth.
Stacey Whitaker
November 7, 2025 AT 06:08Been in Japan for 20 years. Here, they start with MAO-B inhibitors first. No rush to levodopa. They say: ‘Let the brain rest.’ I don’t know if it’s better… but my friend’s mom’s tremors are calmer now. Just saying.
Also-no one talks about how expensive this all is. Even generics. I’m on disability. Paying for patches? Forget it.
Kayleigh Walton
November 8, 2025 AT 13:58For anyone feeling overwhelmed by all these options-take a breath. You’re not behind. You’re not failing. Parkinson’s is a marathon, not a sprint.
Keep a symptom log. Even just a sticky note on the fridge. Note when you feel ‘on,’ when you feel ‘off,’ what you ate, how you slept. Bring it to your neurologist. They’re not judging you-they’re there to help.
And if you’re scared to switch? That’s normal. I was terrified when I moved from Sinemet to Duopa. But my husband held my hand through the surgery. We cried afterward. And then-he ate pancakes with both hands for the first time in 5 years.
You’re not alone. We’re all in this together.
Stephen Tolero
November 9, 2025 AT 03:04What’s the half-life of rotigotine transdermal? And how does its bioavailability compare to oral levodopa under fasting conditions?
Sandridge Neal
November 10, 2025 AT 10:06Thank you for this comprehensive overview. As a neurology nurse with 12 years in movement disorders, I’ve seen patients thrive on Duopa, struggle with Neupro skin reactions, and find unexpected relief with Parcopa. The key is individualization.
One patient, 78, with swallowing issues, went from choking on pills to eating breakfast without fear-just Parcopa. Another, 52, with severe dyskinesia, regained control with Duopa after 6 years of failed oral regimens.
What’s often overlooked: non-pharmacological support. Physical therapy isn’t optional-it’s essential. Speech therapy preserves dignity. Occupational therapy helps with daily tasks. Medication is only one piece.
And yes-generic carbidopa-levodopa is perfectly adequate. There’s no clinical advantage to brand-name Sinemet. Save your money. Invest in therapy, not marketing.
To those considering alternatives: don’t rush. Don’t despair. Work with your team. Parkinson’s evolves. So should your plan. You’re not losing-you’re adapting.
And for the record-CBD oil has no proven benefit in PD. Stick to evidence. Your brain will thank you.