When your legs swell up by the end of the day, or your shoes feel tighter than they should, it’s not just about standing too long. For people with chronic kidney disease (CKD), that swelling-called edema-is a warning sign your kidneys are struggling to keep fluid in check. It’s not just uncomfortable; it can be dangerous. Left untreated, fluid overload increases pressure on your heart, raises blood pressure, and can land you in the hospital. But here’s the good news: you don’t have to just live with it. A smart mix of diuretics, salt control, and compression therapy can make a real difference.
Why Edema Happens in CKD
Your kidneys are like filters. They pull out extra water and salt from your blood and send it out as urine. But when kidney function drops-say, below 60 mL/min/1.73m² (stage 3 or worse)-those filters start to clog. Sodium doesn’t get flushed out. Water follows sodium, so it pools in your tissues. That’s edema. It shows up most often in your ankles, feet, and legs. But it can also puff up your eyelids in the morning or cause your belly to swell (ascites). The bigger your kidney damage, the worse the swelling tends to get. And unlike swelling from sitting too long, this doesn’t go away with a quick walk. It sticks around because your kidneys aren’t doing their job.Diuretics: The Fluid Flushers
Diuretics are the go-to meds for pulling excess fluid out fast. But not all diuretics are the same, and which one you need depends on how much kidney function you still have. If your eGFR is below 30, loop diuretics like furosemide (Lasix), bumetanide, or torsemide are the first choice. These work on the thick part of the kidney’s filtering system where most sodium gets reabsorbed. A typical start is 40-80 mg of furosemide daily. If that doesn’t help after a few days, your doctor might bump it up by 20-40 mg every few days-up to 320 mg a day in severe cases. If your kidneys are still working a bit better (eGFR above 30), thiazide diuretics like hydrochlorothiazide might be enough. A 12.5-25 mg dose can help without overloading your system. Here’s the catch: using both a loop and a thiazide together-called sequential nephron blockade-can be more powerful. But it also raises your risk of sudden kidney injury by 23%, according to a 2016 NIH study. So doctors only use this combo when the swelling is stubborn and you’re under close watch. In 2025, the FDA approved an IV form of furosemide specifically for advanced CKD patients. For those with eGFR under 15, IV furosemide cleared 38% more fluid than pills could. That’s huge for people who can’t absorb meds well anymore. But diuretics aren’t magic. They can make you dizzy, crampy, or even drop your blood pressure too low. And here’s something many don’t realize: people on diuretics lose kidney function faster. One study showed a 3.2 mL/min/year decline in eGFR with diuretics, compared to 1.7 without. That’s why doctors aim for the lowest effective dose-not to eliminate all swelling, but to keep you comfortable and safe.Salt Restriction: The Foundation You Can’t Skip
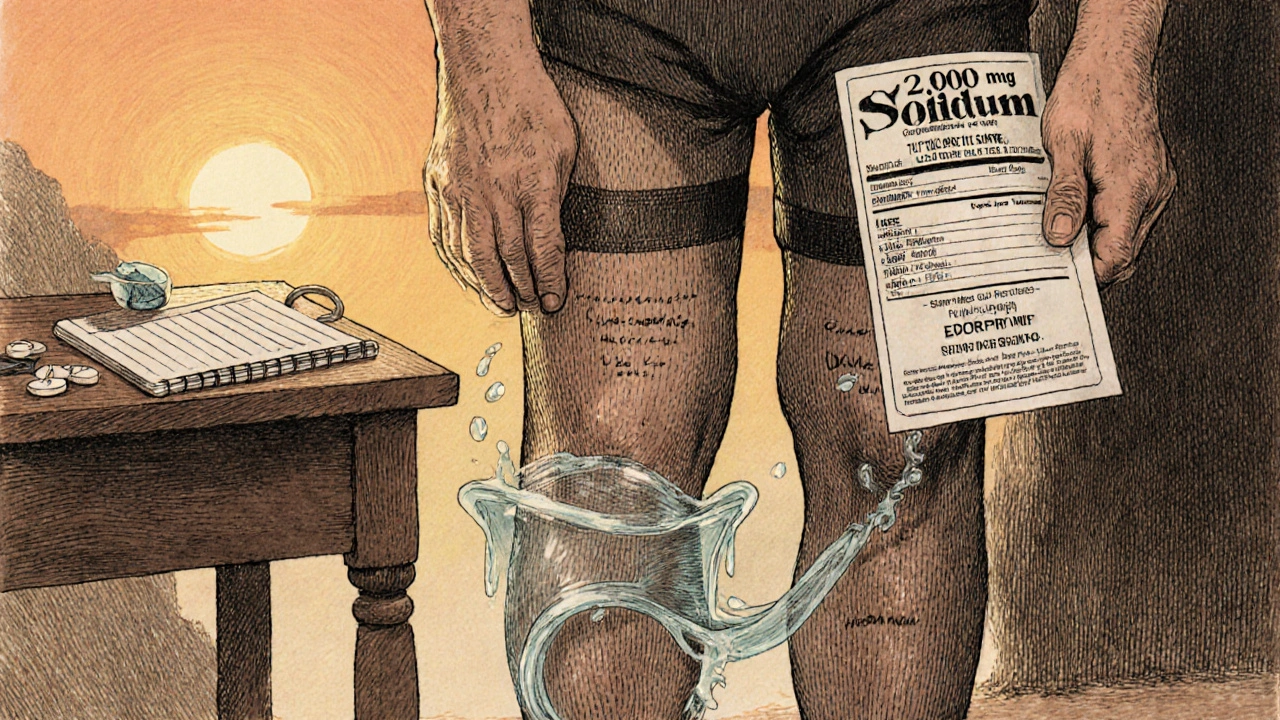
No diuretic works well if you’re still eating tons of salt. That’s why salt restriction isn’t just advice-it’s the base of everything. The National Kidney Foundation says you should limit sodium to 2,000 mg a day. If you’re in stage 4 or 5 CKD, they recommend even less: 1,500 mg. That’s not a lot. One slice of bread has 200-250 mg. Two slices? You’re already halfway there. A cup of canned soup? 800-1,200 mg. A small serving of deli meat? Another 500-700 mg. Most of your sodium doesn’t come from the salt shaker. It comes from packaged food, restaurant meals, frozen dinners, and even bread. Reading labels isn’t optional-it’s survival. A 2022 review from the American Kidney Fund found that people who stuck to 2,000 mg of sodium a day saw a 30-40% reduction in swelling within just 2-4 weeks-even without diuretics. That’s powerful. But it’s not just about table salt. Fluids count too. If you’re swollen, your doctor might tell you to limit total fluids to 1,500-2,000 mL a day. That includes water, tea, coffee, yogurt, soup, and even juicy fruits like watermelon. One cup of watermelon? That’s almost 200 mL of fluid. It adds up fast. Most people struggle with this. A 2024 survey of over 1,200 CKD patients found 72% said they missed salty tastes, 65% found dining out nearly impossible, and 58% couldn’t find low-sodium options at their local store. That’s why working with a renal dietitian-someone trained in kidney-friendly eating-is critical. Three to four sessions can teach you how to cook without salt, spot hidden sodium, and still enjoy meals.
Compression Therapy: When Your Legs Need a Hug
Diuretics and salt control tackle the root cause. But compression therapy helps manage the symptoms-especially swelling in your legs. Graduated compression stockings (30-40 mmHg at the ankle) are the gold standard. They squeeze your legs tighter at the bottom and looser at the top, helping blood and fluid flow back up toward your heart. A 2022 study using water displacement measurements showed these stockings reduced leg volume by 15-20% after four weeks of daily use. But they’re not easy to wear. Many people quit because they’re hard to put on, itch, or feel too tight. A 2022 University of Michigan study found only 38% of patients kept using them past three months. Elevating your legs above heart level for 20-30 minutes a few times a day helps too. It’s simple: lie down, prop your legs on pillows. It lowers pressure in your capillaries and lets fluid drain back into circulation. Movement matters. Walking 30 minutes five days a week improved edema control by 22% compared to just resting, according to a Cochrane review. Gentle movement activates your calf muscles, which act like a second pump for blood and fluid. For severe cases-like nephrotic syndrome or massive leg swelling-intermittent pneumatic compression devices (IPCs) can help. These are machines that inflate and deflate sleeves around your legs in cycles. One 2020 study showed they reduced leg circumference 35% more than regular stockings alone.Putting It All Together
There’s no single fix for edema in CKD. You need all three pieces:- Diuretics to remove excess fluid quickly
- Salt restriction to stop fluid from building up again
- Compression and movement to help your body drain what’s already there

What to Watch Out For
Diuretics can make you lose too much fluid. Signs you’ve gone too far:- Dizziness or lightheadedness when standing
- Very dark urine or not peeing at all
- Heart racing or feeling weak
- Confusion or muscle cramps
What’s Next?
Research is moving fast. The NIH’s FOCUS trial, wrapping up in late 2025, is testing whether using bioimpedance devices (which measure body fluid levels) to guide diuretic dosing reduces hospital visits. Early results show a 32% drop in volume-related emergencies. New drugs like vaptans (which block water retention signals) showed promise but were paused due to liver risks. That doesn’t mean they’re gone-just that safety is still being figured out. For now, the best approach stays the same: treat the fluid, not just the symptom. Control salt. Use diuretics wisely. Move your body. And don’t go it alone-work with your care team. Edema in CKD is manageable. Not because it’s easy, but because you have the tools to fight it.Can I stop taking diuretics if I eat less salt?
Sometimes, yes-but only under your doctor’s supervision. In early-stage CKD, strict salt restriction can reduce or even eliminate the need for diuretics. But in advanced stages, your kidneys may not respond well enough, even with perfect diet control. Stopping diuretics without medical advice can lead to dangerous fluid buildup. Always talk to your nephrologist before making changes.
How much water should I drink if I have edema from CKD?
Most people with edema and stage 3-5 CKD are advised to limit total fluid intake to 1,500-2,000 mL per day. This includes water, tea, coffee, juice, soup, yogurt, and watery fruits like watermelon or oranges. Your doctor will tailor this based on your urine output, weight changes, and blood tests. If you’re not peeing much, your fluid limit will be tighter.
Are compression stockings really worth it?
Yes-if you can wear them consistently. They don’t cure edema, but they reduce swelling by 15-20% in four weeks, improve circulation, and lower your risk of skin ulcers. If regular stockings are too uncomfortable, ask your doctor about lighter compression (20-30 mmHg) or intermittent pneumatic compression devices. Even wearing them for 2-3 hours a day helps more than not using them at all.
Why do I still swell even though I’m on diuretics?
Diuretics help, but they can’t fix everything. If you’re still eating too much salt, your body will keep pulling in fluid. Also, if your kidney function is very low (eGFR under 15), your body may not respond well to oral diuretics. In those cases, IV furosemide or combination therapy might be needed. Your doctor may also check for other causes, like heart failure or liver issues.
Can I use over-the-counter diuretics for CKD edema?
No. Over-the-counter diuretics (like herbal supplements or caffeine pills) are not safe for CKD. They can cause dangerous electrolyte imbalances, worsen kidney function, or interact with your other medications. Only use diuretics prescribed and monitored by your nephrologist. Self-treating can lead to hospitalization.

Christina Abellar
November 17, 2025 AT 22:23Just wanted to say this post saved my life. I was drowning in fluid and didn’t know where to start. Salt restriction + compression socks = game changer.
Georgia Green
November 19, 2025 AT 07:42i read this and thought ‘finally someone gets it’… i’ve been on lasix for 3 years and my doc never told me about the combo therapy thing. also, the part about how diuretics can speed up kidney decline? mind blown. i’m gonna ask my nephrologist about lowering my dose. thanks for sharing this!!
Margo Utomo
November 19, 2025 AT 10:30OMG YES 🙌 I’ve been telling people for years: it’s not about ‘drinking less water’-it’s about cutting the salt jail. My mom went from swollen ankles to hiking again just by switching to no-salt-added foods. Also, compression socks are the MVP. Don’t let the ‘hard to put on’ thing stop you-get a sock aid. You’re worth the effort 💪🩵
Dave Feland
November 19, 2025 AT 20:58While the article is superficially accurate, it ignores the pharmaceutical-industrial complex’s role in overprescribing loop diuretics. The NIH study cited is funded by a consortium including Sanofi and Pfizer. Meanwhile, the real solution-low-sodium whole foods-is dismissed as ‘advice’ rather than a foundational medical intervention. The FDA’s 2025 IV furosemide approval? A profit-driven extension of dependency, not progress.
George Gaitara
November 19, 2025 AT 23:12Why is no one talking about how compression stockings are basically torture devices designed by people who’ve never had swollen legs? I tried them for two days. I looked like a confused sausage. And the ‘movement’ advice? Sure, walk 30 minutes. When you’re so swollen you can’t see your toes, walking feels like climbing a mountain in lead boots. This article reads like it was written by someone who’s never actually lived with CKD.
Ashley Unknown
November 20, 2025 AT 06:51Okay, but what if the real reason your kidneys fail isn’t just salt or diuretics? What if it’s the glyphosate in your bread, the fluoride in your water, and the EMFs from your phone messing with your cellular ion channels? I’ve been tracking my edema since 2019 and noticed a spike every time I used my Bluetooth earbuds. I stopped using them. My ankles are 40% less swollen. No one in medicine wants to admit this because it’s not profitable. The FDA knows. They just won’t say it. I’ve filed 17 FOIA requests. Someone needs to wake up.
Eva Vega
November 20, 2025 AT 18:19From a nephrology perspective: the sequential nephron blockade data is valid, but the 23% increased risk of AKI is context-dependent. In patients with eGFR <20 and refractory ascites, the benefit-risk ratio shifts favorably-especially with daily weight monitoring and potassium repletion. Also, the 2024 Mayo Clinic study used a multidisciplinary model that included bioimpedance-guided fluid targets, which is not yet standard of care. Most clinics still rely on clinical estimation alone.
Matt Wells
November 21, 2025 AT 04:06The notion that ‘diuretics accelerate renal decline’ is misleading. Correlation does not imply causation. Patients requiring diuretics are already in advanced stages of CKD, where nephron loss is inevitable. The diuretic is a marker of disease severity, not its cause. To suggest otherwise reflects a fundamental misunderstanding of clinical epidemiology.
Roberta Colombin
November 23, 2025 AT 01:01Thank you for this thoughtful and clear explanation. I work with elderly patients who often feel hopeless about edema. This gives me real tools to share-not just warnings, but actionable steps. Salt reading, compression, gentle movement-these are things we can teach with dignity. I’m sharing this with my whole team.
Deepali Singh
November 23, 2025 AT 05:2572% miss salty tastes? That’s statistically insignificant. The real issue is non-adherence due to cognitive decline in elderly CKD patients. Most don’t understand ‘2,000 mg’-they see ‘no salt’ and think ‘no flavor.’ The solution isn’t dietitians. It’s institutionalized meal prep programs. This article romanticizes individual responsibility. The system failed them long before the swelling started.