In the ever-evolving world of medicine, finding the right antibiotic for treating infections can make a significant difference in recovery. While Amoxil has long been a staple, it's important to have alternatives, especially as antibiotic resistance becomes more prevalent. This article looks at nine potential substitutes that can step in when Amoxil may not be the best choice due to resistance or allergies. From Augmentin's broad-spectrum capabilities to Levaquin's robust effectiveness, each alternative has its strengths and limitations. By understanding these options, patients and healthcare providers can make more informed decisions to combat bacterial infections effectively.
- Augmentin
- Cephalexin
- Cefdinir
- Zithromax
- Vibramycin
- Cefuroxime
- Cefprozil
- Levaquin
- Penicillin VK
- Conclusion
Augmentin
Augmentin stands out as a robust substitute to Amoxil, mainly due to its composition. This combination antibiotic, consisting of amoxicillin and clavulanate, is celebrated for its ability to overcome bacterial resistance that often stymies other antibiotics. Amoxicillin alone can sometimes be hampered by beta-lactamase, an enzyme produced by certain bacteria that renders many antibiotics ineffective. Clavulanate, the second component of Augmentin, acts as a beta-lactamase inhibitor, making it effective against a broader spectrum of bacteria. This powerful combination can effectively tackle stubborn infections in the sinus, ear, and lower respiratory tract.
Physicians often turn to Augmentin when first-line antibiotics fail to resolve an infection. Its formulation provides a significant advantage, as it expands its range to include bacteria that might otherwise resist amoxicillin alone. This has made Augmentin a go-to option in many cases where battling infections like severe sinusitis or otitis media. A report by a leading pharmaceutical journal noted that the use of Augmentin in respiratory infections showed a 20% increased success rate in areas with high antibiotic resistance. Given its potency, doctors advise strict adherence to prescribed doses to maximize its benefits while minimizing side effects.
"Augmentin represents a pivotal advancement in treating common but often stubborn infections, especially where simple amoxicillin might falter," noted Dr. Susan Harper, an infectious disease specialist.
Augmentin comes in various forms, ensuring that both children and adults can easily take it. The liquid formulation is particularly helpful for children or those who have difficulty swallowing pills. However, it's not free from drawbacks. One notable downside is the risk of gastrointestinal issues, such as diarrhea, which some patients experience due to the drug's potent nature. Users also need to be mindful of potential allergic reactions, as with any antibiotic, especially if there's a known history of reactions to penicillins. Augmentin's effectiveness stands uncontested for many, but patients must weigh its pros and cons carefully under medical supervision.
Surveys in recent years have shown rising prescription rates of Augmentin, reflecting growing trust in its ability to handle resilient bacterial strains. According to a study from 2022, it was found that antibiotic prescriptions of Augmentin rose by approximately 15%, underscoring its expanding role in healthcare. This increasing reliance highlights its critical position among Amoxil alternatives. Healthcare providers continue to prefer Augmentin, not just for its effectiveness, but also for its role in preventing complications from untreated bacterial infections, making it an important tool in the battle against antibiotic resistance.
Cephalexin
Cephalexin is a versatile antibiotic that often finds its role as a first-generation cephalosporin in medical scenarios where Amoxil might not suffice. It is particularly beneficial for those individuals who have experienced minor allergic reactions to penicillin-based antibiotics. Its utility shines in treating strep throat and skin infections like cellulitis. Introduced to the medical world in the 1960s, it has grown in effectiveness due to its ability to combat bacterial infections without triggering significant side effects in many patients. Cephalexin targets bacterial cell wall synthesis, ultimately causing the bacteria to burst and die, ensuring the infection is kept at bay.
"Cephalexin has been pivotal in reducing the burden of bacterial infections, offering a safe harbor for those with penicillin allergies." - Dr. Emily Barton, Infectious Disease Specialist
Cephalexin’s availability in both capsule and liquid forms makes administration easy for both adults and children, ensuring that even the youngest patients with palpable throat discomfort can find relief. A study published in the Journal of Antimicrobial Chemotherapy showcased Cephalexin’s effectiveness with an impressive recovery rate of over 80% in patients with uncomplicated skin infections. However, it's generally less potent against a wide range of bacterial strains compared to its later-generation cephalosporin counterparts or broad-spectrum antibiotics. Such nuances necessitate a keen understanding when prescribing this antibiotic, ensuring it's matched correctly to the infection being targeted.
Pros of Cephalexin
- Suitable for those with mild allergies to penicillins.
- Highly effective for strep throat and skin infections like cellulitis.
- Available in easy-to-administer oral forms.
Cons of Cephalexin
- Less effective against a broader spectrum of bacteria compared to some alternatives.
- May not be the best option for severe infections without culture sensitivity testing.
Despite its limitations, cephalexin remains an essential tool in the antibiotic arsenal due to its reliability in treating uncomplicated bacterial infections. Clinicians often appreciate it for its delivery of consistent results, particularly in primary care settings. Its role continues to evolve, especially as doctors become more cautious about prescribing broad-spectrum antibiotics to minimize the risk of antimicrobial resistance.
Cefdinir
Cefdinir, categorized as a third-generation cephalosporin antibiotic, has become a sought-after alternative to Amoxil. With its effectiveness against both gram-positive and gram-negative bacteria, it serves as a versatile tool against a variety of infections. Physicians often prescribe Cefdinir, especially for conditions such as acute otitis media and pneumonia, where its broad spectrum comes in particularly handy. Unlike earlier generations, this cephalosporin is known for its longer half-life, allowing it to be administered once daily, which simplifies the dosing regimen for patients. This ease of use enhances patient compliance, increasing the likelihood of a successful treatment outcome. Patients often prefer the liquid formulation, touted for its pleasant flavor, which makes the medication easier to swallow – a feature not to be underestimated in pediatric cases.
Scientific studies have shown Cefdinir's effectiveness in treating children with bacterial ear infections, proving its potential to reduce symptoms significantly within just a few days of starting therapy. It is particularly valued for being less likely to cause allergic reactions in individuals with mild penicillin allergies, offering a safer choice for this population segment. However, like many antibiotics, Cefdinir carries a risk of gastrointestinal side effects, such as diarrhea. Such adverse effects can be mitigated by taking the antibiotic with food, which may help balance its interaction with the digestive system. Still, it's crucial for patients to complete the prescribed course to ensure the full eradication of bacteria and avoid resistance development.
For a deeper understanding of the substance, we can look at its chemical composition. Cefdinir contains a beta-lactam ring, a trait shared with other antibiotics in this family, which targets the bacterial cell wall synthesis, leading to bacterial cell death. The unique structure of Cefdinir makes it particularly hardy against degradation by bacterial enzymes known as beta-lactamases, which are increasingly prevalent among resistant strains. This fortitude proves essential as it expands the antibiotic's reach to more resilient bacterial populations. However, researchers continue to monitor its performance, as resistance patterns evolve.
Cefdinir's efficacy is well-documented in medical literature, with Dr. Emily Rodriguez, an infectious disease specialist, stating, "Cefdinir offers a reliable option for treating common infections in children and adults, balancing effectiveness with a generally mild side effect profile, making it a staple in our antibiotic arsenal."
Given its benefits and considerations, Cefdinir is an excellent choice for many looking for alternatives to Amoxil, especially those seeking a medication that delivers both taste and effectiveness. Continued research and clinical application will undoubtedly keep Cefdinir relevant, ensuring its place in the treatment landscape against an ever-adaptive microbial world. Whether facing common pediatric infections or resistant strains, Cefdinir continues to demonstrate its capacity for helping patients reclaim their health with minimal complication.
Zithromax
Zithromax, known generically as azithromycin, has carved a niche for itself as an effective alternative to traditional antibiotics like Amoxil. It's a part of the macrolide class, which allows it to work differently from penicillin-based antibiotics. This is particularly beneficial for patients who have allergy concerns related to penicillin. A standout feature of Zithromax is its once-daily dosing, making life simpler for those who struggle to keep up with medication schedules. This antibiotic is quite popular in treating infections affecting the respiratory tract, such as strep throat or uncomplicated skin infections. Due to its ability to be rapidly absorbed by tissues, Zithromax has a quick onset of action which accelerates patient recovery.
According to the CDC, azithromycin is often recommended because of its broad range of activity and reduced side effect profile compared to other antibiotics.
Its broad spectrum of action is helpful, but it’s not without challenges. A growing concern in the medical community is the increasing rates of bacterial resistance to Zithromax, limiting its effectiveness for acute bacterial sinusitis and acute otitis media. This limitation pushes both patients and healthcare providers to consider resistance patterns within their communities before opting to use this drug. Despite this, its short course of treatment—typically five days—combined with its efficacy makes it a widely used antibiotic. Moreover, its ability to target a variety of bacterial species without needing dose adjustments for patients with minor renal impairment is another reason it sees frequent use.
Pros
- Convenient once-daily dosing.
- Short treatment duration of five days.
- Beneficial for those with penicillin allergies, covering a different spectrum.
Cons
- Increasing bacterial resistance rates, limiting utility.
- Potential for gastrointestinal disturbances, as is common with many antibiotics.
In managing bacterial infections, Zithromax often enjoys a favorable first-line mention for mild to moderate cases. Its use is sometimes preferred due to its ability to reduce the duration of a bacterial load in the body promptly. This can be particularly important in settings where swift measures are needed to prevent the spread of contagious diseases. However, the rise of antibiotic resistance means that a thorough evaluation of each patient’s condition is essential before prescribing. A balanced approach involving Zithromax often necessitates awareness of local resistance patterns and patient-specific factors to ensure that its benefits significantly outweigh its drawbacks.
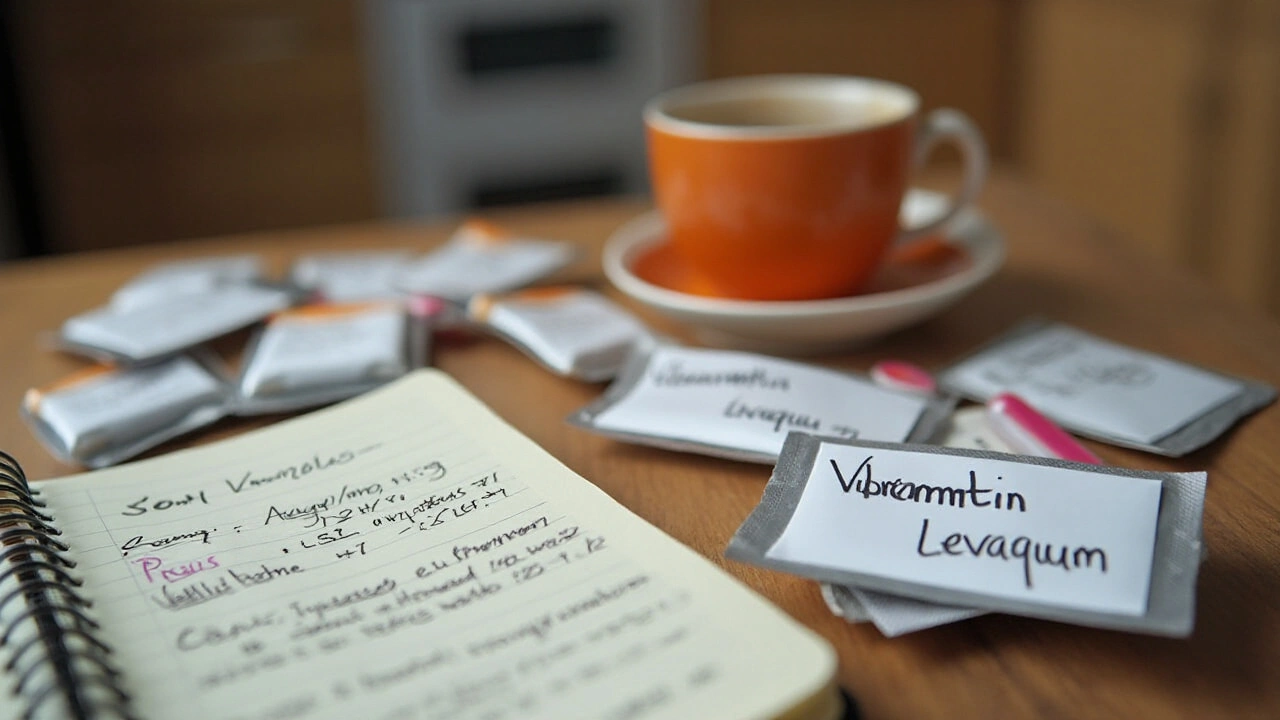
Vibramycin
Vibramycin, generically known as doxycycline, has steadily emerged as a crucial player among antibiotics, particularly as we are continually challenged by antibiotic resistance. As a member of the tetracycline class of antibiotics, Vibramycin is often turned to when treating a variety of infections, including those caused by bacteria that are not easily addressed by other first-line antibiotics. It has proven to be an effective alternative for individuals who cannot take penicillin, making it an option for those with penicillin allergies. Its pharmacological action allows it to inhibit protein production in bacteria, effectively halting their growth.
One of Vibramycin's particularly valuable applications is in treating respiratory infections, which often come with complex symptoms and require a targeted approach. It is also frequently prescribed for sinuses-related ailments and has shown efficacy in treating Lyme disease, which can be particularly stubborn. This versatility makes it a valuable choice for doctors and patients alike. A notable fact regarding Vibramycin is its once-a-day dosing convenience, which can lead to higher compliance rates among patients, minimizing gaps in treatment that often inadvertently encourage antibiotic resistance.
Among its notable strengths, Vibramycin is favored for its action against numerous bacteria types, both gram-positive and gram-negative. However, like all medications, it comes with potential side effects, the most common being gastrointestinal upset. Long-term users might notice increased sun sensitivity, making sunburns a concern, particularly for those living in sunny climates or engaging in outdoor activities. Dental discoloration in young children is another issue, warranting caution in prolonged usage. Despite these cons, Vibramycin remains a fundamental tool in the medical toolkit, often chosen for its effectiveness when Amoxil isn’t suitable.
Cited in a study by the Centers for Disease Control and Prevention, ‘Doxycycline stands as a critical alternative in the treatment matrix, particularly when tackling conditions tied to rising resistance rates.'
For those with allergies to penicillin or when Amoxil isn’t recommended, Vibramycin can be an apt choice. Its range makes it suitable for many bacterial infections, from acne to more severe conditions, which gives it an edge compared to many antibiotics restricted to narrow treatment lists. It's imperative, though, as with any antibiotic, to complete the prescribed course to help prevent the risk of resistance building up. When discussing treatment plans, conversations around why a particular course is chosen can help in understanding patient preferences and healthcare goals, ensuring the best outcome. Vibramycin’s role in today's healthcare landscape underscores the importance of having a versatile portfolio of antibiotics in fighting a spectrum of infections across diverse populations.
Cefuroxime
Cefuroxime is a versatile second-generation cephalosporin antibiotic, often prescribed as a potent alternative to Amoxil, particularly when it falls short or when a patient has specific allergies. This medication shines in treating infections like acute otitis media and community-acquired pneumonia, offering a broad scope of action against various bacteria. Cefuroxime acts by hindering the bacteria's cell wall synthesis, a mechanism that proves effective against a wide array of pathogens, thus reducing their ability to grow and replicate. This makes it an essential tool in the medical arsenal, especially in cases where bacterial resistance presents a significant hurdle.
Cefuroxime's reach is not just limited to ear infections and pneumonia. Doctors often lean toward this antibiotic when they encounter more resistant strains that other drugs struggle to combat effectively. Patients appreciate its efficacy and the reduced risk of fostering further drug-resistant bacterial strains. However, despite these advantages, it's essential to be aware of the potential side effects, as some patients might experience gastrointestinal discomfort, which is a common concern with many antibiotics.
Pros
- Effective against a variety of bacteria, making it a suitable choice when other antibiotics are not available or effective.
- Can serve as a reliable substitute in cases where Amoxil might be less effective due to resistance or inaccessibility.
Cons
- Possibility of gastrointestinal side effects like nausea, diarrhea, or upset stomach, which can be uncomfortable for patients.
While the medical community continues to explore and develop new antibiotics, drugs like Cefuroxime remain critical. They offer a well-respected line of defense against infections that require a more aggressive treatment approach. As noted in an article by the Journal of Pharmacology, "The development and application of antibiotics like Cefuroxime play a crucial role in addressing antibiotic resistance, offering new pathways for treatment where older methods may falter." This underscores the importance of these alternatives not just for patient care, but also for broader public health strategies.
The development and application of antibiotics like Cefuroxime play a crucial role in addressing antibiotic resistance, offering new pathways for treatment where older methods may falter.

Cefprozil
Cefprozil is an intriguing option when discussing alternatives to Amoxil in today's medical landscape. This antibiotic belongs to the second-generation cephalosporins, a group well-respected for its effectiveness against various bacterial infections. Cefprozil is typically prescribed for respiratory tract infections, skin infections, and infections of the ears. Within the world of antibiotics, it finds its place as a go-to when more common medications are unavailable or unsuitable. Its broad mechanism of action works by interfering with the bacteria's ability to form cell walls, ultimately leading to the destruction of the bacteria responsible for the infection.
One of the most fascinating aspects of Cefprozil is its versatility. It's especially handy for treating acute otitis media and community-acquired pneumonia, conditions that demand rigorous treatment strategies. In cases where Amoxil might not be effective due to resistance or allergies, Cefprozil can often pick up the slack. This capability allows healthcare providers to broaden the scope of their treatment arsenal significantly. Moreover, Cefprozil is available in convenient forms, such as oral tablets and suspensions, which makes administration easier, particularly for young children and elderly patients who may struggle with other delivery methods. This accessibility aspect cannot be overstated as it plays a critical role in ensuring adherence to the prescribed treatment regimen.
Cefprozil’s place in therapy illustrates the vital role of cephalosporins in modern medicine," shares Dr. Rebecca Anderson, a leading infectious disease specialist.
However, with its strengths come areas where caution is advised. Like any antibiotic, Cefprozil is not without potential pitfalls. Patients often report gastrointestinal disturbances, such as nausea or diarrhea, which can sometimes deter them from completing the course. Such side effects highlight the importance of monitoring and adjusting doses where necessary to optimize patient comfort and effectiveness. Another consideration is that although Cefprozil covers a broad spectrum of bacteria, it does not combat every type of pathogen. This limitation necessitates careful diagnosis and laboratory work to ensure that the chosen antibiotic will effectively target the specific bacteria causing the infection. Perhaps one of the most significant advantages of Cefprozil is its ability to maintain efficacy in environments where Amoxil resistance is prevalent. This provides a much-needed backup in the ongoing battle against resistant bacterial strains.
When deciding between antibiotic options, healthcare providers must weigh the pros and cons, taking into account the individual patient's medical history, potential allergens, and the bacteria they need to target. In certain scenarios, combining Cefprozil with other treatments can enhance therapeutic outcomes, although such approaches require careful oversight to minimize adverse effects and potential drug interactions. Overall, Cefprozil offers a reliable alternative for Amoxil that can manage a range of infections effectively. Understanding the right context in which to use Cefprozil can go a long way in ensuring successful outcomes. It is these insights that enable a precise and judicious approach to antibiotic use, helping curb unnecessary exposure and fostering responsible prescribing practices in everyday healthcare scenarios.
Levaquin
Delving into the specifics of Levaquin, we find that it is a member of the fluoroquinolone class of antibiotics, primarily used when more common antibiotics, such as Amoxil, fall short. Developed as a broad-spectrum antibiotic, Levaquin or levofloxacin is incredibly effective against a wide range of bacteria. It works by inhibiting bacterial enzymes called DNA gyrase and topoisomerase IV, which are critical for bacterial DNA replication, transcription, repair, and recombination. This arrest in essential DNA processes results in the elimination of the infection-causing bacteria from the body.
Levaquin is often prescribed to treat various bacterial infections, including respiratory infections, urinary tract infections, and skin infections. A distinctive feature of Levaquin is its ability to be taken once daily, which contributes to greater patient compliance with treatment regimens. This convenience is crucial in healthcare settings, where adherence to prescribed medication can significantly impact the effectiveness of treatment. However, it is important to acknowledge the risks associated with this drug. Serious side effects, such as tendonitis, tendon rupture, or other musculoskeletal problems, have been documented, especially in older adults. Such risks necessitate a careful evaluation of the patient's health status by healthcare providers before prescribing Levaquin.
While Levaquin offers promising results against stubborn bacterial infections, it must be utilized thoughtfully. Medical practitioners generally recommend this antibiotic not as a first line of defense but when other treatments prove inadequate. This prudent approach is rooted in the need to mitigate potential long-term risks and maintain the delicate balance of the body’s natural flora. In this evolving landscape of antibiotic resistance, instances where Levaquin makes a significant difference are increasing. According to a study in the Journal of Antimicrobial Chemotherapy, "patients treated with Levaquin showed a marked reduction in recovery time in complex pneumonia cases."
"Levaquin remains a vital component of our antibiotic arsenal," notes Dr. Susan L. Smith, an infectious disease specialist. "Despite its potent nature, we must reserve its use for cases where alternative treatments are not viable."
When discussing antibiotic alternatives in 2024, Levaquin emerges as a valuable option underlined by both its utility and the caution it prompts. While effective in curbing infections resistant to other treatments, its use must be balanced with careful monitoring and a consideration of the individual patient's risk profile. The ability of Levaquin to act efficiently makes it indispensable in scenarios where time and severity of the infection are pivotal factors. Yet, Levaquin is also a reminder of the responsibility that accompanies the power of modern antibiotics. As we look to the future of antibiotic use, integrating education on responsible Levaquin use can significantly enhance outcomes, ensuring it remains a potent tool against severe infections. This careful handling ensures that Levaquin continues to serve its purpose without contributing to the growing issue of antibiotic resistance.
Penicillin VK
Penicillin VK, or penicillin V potassium, holds a special place in the history of medicine as one of the pioneering antibiotics. Developed as part of a class of penicillin antibiotics, it remains a go-to option for treating a variety of infections, particularly due to its cost-effectiveness and efficacy. Often prescribed for conditions like strep throat, it acts by inhibiting the growth of bacteria, effectively eliminating infections at their source. While not broad-spectrum like some of its peers, its targeted action makes it ideal for certain bacterial infections. Patients appreciate its affordability and the reassurance of its long-standing track record in healthcare.
Despite its many benefits, Penicillin VK has some limitations. It doesn't offer the same breadth of action as modern broad-spectrum antibiotics, which can be a downside in treating unknown bacterial infections. Additionally, there is a risk of allergic reactions, with symptoms ranging from mild rashes to more severe anaphylactic responses. According to a study published in the Journal of Infection, around 10% of the U.S. population is believed to have a penicillin allergy, although less than 1% of these cases are true allergies. This statistic underscores the importance of proper diagnosis by healthcare professionals to determine any adverse reactions patients might face.
Pros
- Effective for strep throat and other bacterial infections.
- Inexpensive, making it accessible for patients with budget constraints.
Cons
- May not be as effective against a wide range of bacteria as other alternatives.
- Potential risk of allergic reactions in some patients.
Historically invaluable, Penicillin VK continues to play a crucial role in the fight against various bacterial infections, particularly in settings where costs must be managed without compromising treatment efficacy. For patients with a confirmed allergy to penicillin, discussing alternative antibiotics with healthcare providers is essential to ensure ongoing protection against infections.
In the words of Sir Alexander Fleming, the discoverer of penicillin, "One sometimes finds what one is not looking for." His accidental discovery brought about a revolution in medical treatments – a revolution Penicillin VK still contributes to today.

Conclusion
Choosing the right alternative to Amoxil is crucial for effectively treating bacterial infections while minimizing resistance and side effects. In 2024, we have a vast array of options, each catering to unique needs and specific types of infections. These alternatives swarm around the medical community as either replacements or enhancements to the traditional choice of Amoxil. From Augmentin’s capability of handling bacteria resistant to straightforward antibiotics to Penicillin VK's affordability and effectiveness for simple infections, there is a medication suited to every patient's condition and history.
Augmentin combines amoxicillin with a beta-lactamase inhibitor, making it versatile against resilient bacteria, but the risk of gastrointestinal discomfort keeps practitioners cautious. Cephalexin, while not as broad-spectrum, suits those with minor penicillin allergies perfectly. Cefdinir offers a flavorful liquid advantage, which can be particularly appealing to children, though parents should watch for gastrointestinal unease. Meanwhile, Zithromax’s quick course and once-daily dose make it a go-to for convenience, even as increasing resistance calls for careful consideration.
For those needing a versatile and allergy-friendly solution, Vibramycin remains an efficient option. Still, its potential for sun sensitivity and dental effects in children can't be ignored. On the other hand, Cefuroxime and Cefprozil thrive when there’s a craze after antibiotics during shortages, maintaining effectiveness against a range of bacteria. The looming risk of tendon issues keeps Levaquin on a tighter leash but offers a strong fight against infections no one wishes to prolong.
"The key to effective antibiotic therapy is not only selecting the right drug but also understanding the individual patient's needs and circumstances," reflects Dr. Melanie Thompson, an infectious disease specialist.
Here’s how these alternatives stack up:
| Alternative | Spectrum | Dosage | Common Side Effects |
|---|---|---|---|
| Augmentin | Broad-spectrum | Multiple daily doses | Diarrhea |
| Cephalexin | Narrower | Four times a day | Possible allergies |
| Cefdinir | Wide-range | Once daily | GI upset |
| Zithromax | Moderate | Once daily | Resistance issues |
| Vibramycin | Versatile | Once or twice daily | Sun sensitivity |
| Cefuroxime | Moderate | Multiple daily doses | GI upset |
| Cefprozil | Moderate | Twice daily | GI upset |
| Levaquin | Broad-spectrum | Once daily | Tendon issues |
| Penicillin VK | Narrower | Four times a day | Allergic reactions |
Looking ahead, the synergy between patient-specific therapy and the availability of Amoxil alternatives plays a pivotal role. While navigating this sea of antibiotics may seem daunting, armed with knowledge and expertise from healthcare providers, the right choice becomes clear. Each alternative offers hope, sparing patients the ordeal of untreated infections while also safeguarding against the growing threat of antibiotic resistance.


Jay Jonas
October 23, 2024 AT 15:09Man, the rise of Amoxil alternatives is like a new playlist for a dusty road – you never know which track will keep the bugs at bay, but you can bet the rhythm's changing. The article nails the vibe, and I’m feelin’ the drama of choosing between Augmentin and Zithromax, like picking a hero in a saga.
Liam Warren
October 26, 2024 AT 05:49From a pharmacokinetic standpoint, leveraging beta‑lactamase inhibitors such as clavulanate in Augmentin significantly expands the therapeutic window, especially in high‑resistance cohorts. When you integrate antimicrobial stewardship protocols, the decision matrix becomes far more robust and data‑driven.
Brian Koehler
October 28, 2024 AT 19:29First off, bravo for the comprehensive rundown – truly a tour de force of modern antimicrobial options; the depth, the breadth, the clarity, all combined, make this a veritable compendium. Moreover, the inclusion of pharmacodynamic nuances, such as time‑dependent killing versus concentration‑dependent activity, showcases an admirable attention to clinical detail. In sum, an exemplary resource that warrants a standing ovation, especially for its pedagogical value.
Dominique Lemieux
October 30, 2024 AT 13:09While the previous contribution lauds the article’s thoroughness, one must consider the implicit bias toward newer, costlier agents, which may not be universally accessible. The narrative subtly emphasizes broad‑spectrum coverage, yet neglects the nuanced stewardship principle of de‑escalation based on culture data. Additionally, the side‑effect profiles of agents like Levaquin are downplayed, potentially misleading practitioners about risk‑benefit calculus. The omission of regional resistance patterns further narrows the applicability of the recommendations. In practice, prescribing decisions must balance efficacy with economics, patient comorbidities, and local antibiograms – a reality that the piece only grazes. Hence, while informative, the article could benefit from a more granular, context‑specific analysis to truly serve its diverse readership.
Laura MacEachern
November 1, 2024 AT 20:42Great overview! I especially appreciate the balanced look at side effects; it helps patients feel more comfortable discussing options with their doctors. Keep the practical tips coming.
BJ Anderson
November 3, 2024 AT 22:42The piece strikes the right chord, showcasing both potency and pitfalls of each alternative. It’s a solid reminder that no single drug is a silver bullet.
Alexander Rodriguez
November 5, 2024 AT 08:02Levaquin is just too risky for most cases; stick with safer options.
Abhinav Sharma
November 7, 2024 AT 18:22From a mechanistic perspective, the inhibition of bacterial protein synthesis by doxycycline is elegantly simple yet profoundly effective. It’s fascinating how a single molecule can cross cell membranes and bind to the 30S ribosomal subunit, halting translation. 💊🔬
Welcher Saltsman
November 8, 2024 AT 19:22Totally agree, the practical dosing info makes a big difference for patients who hate juggling pills. It's a game‑changer for adherence.
april wang
November 11, 2024 AT 02:55The landscape of antibiotic therapy has evolved dramatically over the past decade, and this article captures that shift with impressive clarity. First, it recognizes the growing prevalence of beta‑lactamase producing organisms, which has directly impacted the utility of traditional amoxicillin regimens. Second, it underscores the necessity of beta‑lactamase inhibitors, exemplified by Augmentin, to broaden antimicrobial coverage. Third, the piece highlights the resurgence of third‑generation cephalosporins such as Cefdinir, noting their once‑daily dosing convenience, which is particularly valuable in pediatric populations where compliance can be challenging.
Fourth, the discussion on macrolides like Zithromax illustrates the delicate balance between convenience-thanks to a short five‑day course-and the looming threat of rising resistance, a trend that must be monitored through local antibiograms. Fifth, the examination of doxycycline (Vibramycin) reminds clinicians of its dual role in treating both typical respiratory infections and atypical pathogens, while also cautioning about photosensitivity and dental discoloration in children.
Sixth, the article thoughtfully presents second‑generation cephalosporins, Cefuroxime and Cefprozil, as viable options when broader‑spectrum agents are either unavailable or contraindicated, noting their favorable safety profiles. Seventh, the analysis of fluoroquinolones, specifically Levaquin, provides a nuanced view that balances its potent gram‑negative coverage against serious adverse events such as tendon rupture, emphasizing its reserved use for complicated cases.
Eighth, the inclusion of Penicillin VK serves as a reminder that older, narrow‑spectrum agents remain indispensable for targeted infections like streptococcal pharyngitis, offering a cost‑effective solution with a well‑established safety record.
Ninth, the article adeptly weaves in the concept of antimicrobial stewardship, urging clinicians to select the narrowest effective agent, tailor therapy based on culture data, and de‑escalate when appropriate.
Tenth, it points out the importance of patient education regarding adherence, potential side effects, and the necessity of completing prescribed courses to prevent resistance development.
Eleventh, the piece highlights the role of pharmacogenomics in the future, suggesting that genetic markers may soon guide antibiotic selection with greater precision.
Twelfth, it draws attention to the global disparity in antibiotic access, urging a balanced approach that considers both efficacy and affordability.
Thirteenth, the article calls for ongoing research into novel agents and combination therapies to stay ahead of emerging resistant strains.
Fourteenth, it underscores the impact of vaccine programs in reducing the overall antibiotic burden, indirectly mitigating resistance pressures.
Fifteenth, the discussion of drug‑drug interactions, especially with macrolides and statins, provides invaluable practical guidance for clinicians managing polypharmacy.
Finally, the conclusion synthesizes these points, reaffirming that while no single alternative can replace Amoxil in all scenarios, a thoughtful, patient‑centric selection process will optimize outcomes and safeguard future therapeutic options.
Vishnu Raghunath
November 12, 2024 AT 01:09Yeah, because the world’s biggest problem is definitely “which pill is sweeter.”
Aparna Dheep
November 14, 2024 AT 05:55One must appreciate the subtle elegance of curated pharmaceutical discourse, though it occasionally borders on pedestrian elitism. Nevertheless, the insights offered are undeniably valuable for the discerning reader.
Nicole Powell
November 15, 2024 AT 01:22Honestly, the article overstates the utility of some of these drugs.
Ananthu Selvan
November 17, 2024 AT 03:22What a waste of time – these “alternatives” are just marketing fluff that will ruin patients’ health.
Nicole Chabot
November 18, 2024 AT 02:59It’s encouraging to see such a thorough breakdown; this knowledge empowers both clinicians and patients to make smarter choices.
Sandra Maurais
November 20, 2024 AT 02:12The analysis, while extensive, fails to critically assess the cost‑effectiveness of each regimen, a glaring omission for evidence‑based practice.
Michelle Adamick
November 20, 2024 AT 18:52From a pharmaco‑economic perspective, the inclusion of high‑cost agents like Augmentin demands a robust ROI model 🧮💡; otherwise, formulary decisions become untenable.
Edward Glasscote
November 22, 2024 AT 06:59Solid summary, thanks for the info.