Flu Complication Risk Calculator
Personal Risk Assessment
Enter your information to get a personalized assessment of your risk for flu complications.
Every year the flu hits hard, but most people assume a mild fever and a sore throat are the end of the story. In reality, flu complications can turn a simple illness into a serious health threat, especially for vulnerable groups. This guide explains what to watch for, why certain people are at higher risk, and practical steps to keep the infection from spiraling out of control.
What is influenza?
Influenza is a highly contagious respiratory virus that spreads through droplets when an infected person coughs, sneezes, or talks. It belongs to the Orthomyxoviridae family and exists in three main sub‑types-A, B and C-each with its own strain variations. Typical incubation lasts 1‑4 days, symptoms peak around day 2, and most healthy adults recover within a week.
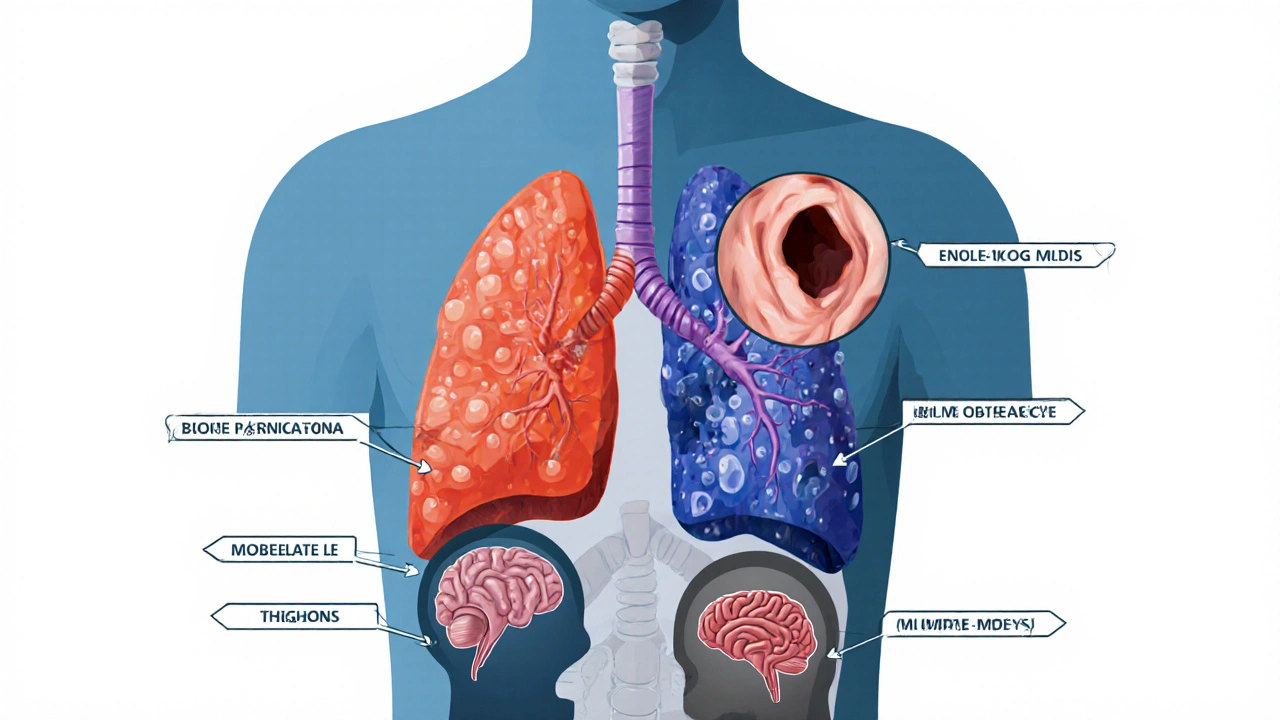
Common complications that can arise
While many recover without incident, the virus can set off a chain reaction in the body, leading to secondary problems. Below are the most frequently reported complications:
- Pneumonia - A bacterial infection that settles in the lungs after the virus weakens the airway defenses. It’s the leading cause of flu‑related hospitalizations.
- Sinusitis - Inflammation of the sinus cavities that can cause facial pain and prolonged congestion.
- Otitis media - Middle‑ear infections, especially common in children, that cause pain and hearing loss.
- Myocarditis - Inflammation of the heart muscle, which can lead to arrhythmias or heart failure in severe cases.
- Encephalitis - Rare but serious brain inflammation presenting with confusion, seizures, or loss of consciousness.
- Exacerbation of chronic asthma or COPD - The virus irritates already inflamed airways, increasing breathing difficulty.
- Severe dehydration - High fever and rapid breathing can deplete fluids quickly, especially in infants and the elderly.
- Secondary bacterial infection - Bacteria such as Streptococcus pneumoniae or Staphylococcus aureus take advantage of damaged mucus membranes.
These complications don’t appear out of nowhere; they follow a pattern of weakened immunity, damaged tissue, and bacterial colonisation. Understanding the sequence helps you intervene early.
Who is most likely to develop complications?
Age, health status, and lifestyle all influence the risk. The table below summarises the groups that need extra vigilance.
| Risk group | Why they’re vulnerable | Common complications |
|---|---|---|
| Adults >65 years | Weaker immune response, pre‑existing heart or lung disease | Pneumonia, myocarditis, dehydration |
| Children <5 years | Immature immune system, narrow airways | Otitis media, sinusitis, pneumonia |
| Pregnant women | Altered immunity, increased respiratory demand | Pneumonia, severe dehydration |
| People with chronic conditions (asthma, COPD, diabetes, heart disease) | Baseline inflammation, medication interactions | Exacerbation of disease, pneumonia, myocarditis |
| Immunocompromised (cancer therapy, organ transplant, HIV) | Reduced ability to fight viral and bacterial invaders | Secondary bacterial infection, encephalitis |
Warning signs that a complication is developing
Most flu symptoms fade after a few days. If you notice any of the following, it’s time to act:
- Persistent high fever (>101°F / 38.3°C) lasting more than 3-4 days.
- Shortness of breath, wheezing, or chest pain that wors’t with rest.
- Sudden worsening of cough with yellow‑green sputum.
- Severe headache, neck stiffness, or confusion.
- Ear pain that doesn’t improve within 48hours.
- Rapid heart rate, dizziness, or fainting spells.
- Decreased urination, dry mouth, or feeling light‑headed-signs of dehydration.
These red flags indicate that influenza has either damaged tissue or invited a secondary infection. Prompt medical evaluation can prevent hospitalisation.
Prevention: How to keep complications at bay
Stopping the flu before it starts, or catching it early, is the most effective way to avoid nasty sequelae.
- Vaccination - An annual flu shot reduces the risk of severe disease by up to 60% and cuts hospital admissions for complications dramatically.
- Early antiviral therapy - Prescription drugs like oseltamivir (Tamiflu) work best when started within 48hours of symptom onset. They shorten the illness by about a day and lower the chance of pneumonia.
- Hand hygiene - Washing hands with soap for at least 20seconds removes viral particles. Alcohol‑based sanitiser is a good backup.
- Respiratory etiquette - Cover sneezes with a tissue or elbow, and discard tissues promptly.
- Stay hydrated and rest - Fluids thin mucus, making it easier for the immune system to clear the virus.
- Manage chronic conditions - Keep asthma inhalers, diabetic meds, and heart drugs up‑to‑date; uncontrolled disease heightens complication risk.
- Avoid smoking and exposure to air pollutants - These irritants further damage the airway lining.
For high‑risk individuals, a doctor may recommend a higher‑dose vaccine or an additional booster, especially in years when the circulating strain is aggressive.
What to do if a complication occurs
Even with the best precautions, complications can still arise. Here’s a practical plan:
- Seek medical attention immediately if you experience any warning signs listed above.
- Ask for a chest X‑ray if pneumonia is suspected; it confirms lung involvement.
- If a bacterial infection is confirmed, a course of antibiotics (e.g., amoxicillin or azithromycin) is typically prescribed for 5-7days.
- For heart‑related issues like myocarditis, cardiology evaluation and possibly anti‑inflammatory medication are needed.
- Encephalitis requires urgent neuro‑imaging (CT/MRI) and intravenous antiviral therapy, often in a hospital setting.
- Supportive care - Intravenous fluids for dehydration, supplemental oxygen for breathing difficulties, and pain relief for ear or sinus pain.
- Follow‑up - A repeat visit after 48-72hours ensures the complication is responding to treatment.
Documenting symptom progression (temperature chart, cough frequency) can help clinicians tailor treatment quickly.

Everyday habits that boost recovery and guard against complications
When you’re already sick, small lifestyle tweaks make a big difference.
- Drink warm fluids (herbal tea, broth) every 2hours to keep mucus thin.
- Use a humidifier at night to soothe irritated airways.
- Eat protein‑rich foods (lean meat, legumes, yogurt) to support immune cell production.
- Avoid alcohol and caffeine, which can worsen dehydration.
- Take over‑the‑counter pain relievers (paracetamol or ibuprofen) only as directed to control fever and aches.
- Rest on a comfortable, slightly elevated mattress to ease breathing.
- If you have asthma, continue inhaler use as prescribed; don’t skip doses because you feel ‘better’.
These habits keep the body’s defenses strong enough to finish clearing the virus before secondary bacteria take hold.
Quick takeaways
- Influenza can lead to pneumonia, sinusitis, otitis media, myocarditis, encephalitis, and more.
- Adults over 65, young children, pregnant women, and anyone with chronic disease are most at risk.
- Persistent fever, breathing trouble, worsening cough, or confusing symptoms signal a complication.
- Annual flu vaccination, early antivirals, and good hygiene cut the chance of severe outcomes.
- If you notice warning signs, see a doctor fast-early treatment saves lives.
Frequently Asked Questions
Can the flu cause heart problems?
Yes. Influenza can inflame the heart muscle, a condition called myocarditis. Symptoms include chest pain, shortness of breath, and palpitations. If you have a pre‑existing heart condition, the risk is higher, and you should contact a healthcare provider promptly if you notice these signs.
How long after flu symptoms start should I wait before starting antivirals?
Antiviral medication works best when begun within 48hours of the first fever or cough. Starting later can still help high‑risk patients, but the benefit diminishes. Talk to your doctor as soon as you suspect the flu.
Is it safe to take a flu vaccine during pregnancy?
Absolutely. The inactivated flu shot is recommended for all pregnant women, regardless of trimester. It protects both mother and baby from severe flu complications and has a strong safety record.
What distinguishes viral pneumonia from bacterial pneumonia?
Viral pneumonia often follows a flu infection and shows up as diffuse, “ground‑glass” infiltrates on a chest X‑ray, with a slower onset. Bacterial pneumonia usually presents suddenly with high fever, purulent sputum, and localized lobar consolidation on imaging. Doctors may order sputum cultures to confirm the cause.
Can dehydration worsen flu complications?
Yes. Dehydration reduces mucus fluidity, making it harder for the body to clear the virus and any secondary bacteria. It also strains the heart and kidneys, especially in older adults. Maintaining regular fluid intake is a simple yet critical preventive measure.


Richard Wieland
October 12, 2025 AT 06:17I’m sorry to hear many people suffer from flu complications. Stay vigilant and seek help early if symptoms worsen.
rachel mamuad
October 13, 2025 AT 01:43Yo, this flu thing is def a major public‑health concern, especially w/ the comorbidities u mentioned. Gotta keep an eye on dem risk scores, lol.
Maricia Harris
October 13, 2025 AT 21:10Honestly, this whole guide feels like a horror movie for the elderly!
Tara Timlin
October 14, 2025 AT 16:37Great rundown! If you’re high‑risk, start antivirals within 48 hours – it can shave a day off the illness and cut pneumonia risk. Also, keep a log of temperature and symptoms; it helps doctors spot complications early. Hydration and rest are non‑negotiable, especially for seniors.
benjamin malizu
October 15, 2025 AT 12:03One must recognize that dismissing flu prophylaxis constitutes a flagrant neglect of communal responsibility; such cavalier attitudes exacerbate morbidity and mortality rates across susceptible demographics.
Maureen Hoffmann
October 16, 2025 AT 07:30Hey, I get the moral high‑ground vibe, but let’s turn that into action! Remember, staying on top of vaccinations, hydration, and early antivirals isn’t just selfish – it’s a community service. Keep the encouragement flowing, and don’t let guilt freeze you out.
Alexi Welsch
October 17, 2025 AT 02:57While the article highlights vaccination, it neglects to address the variable efficacy observed in antigenic drift seasons, which can leave even the vaccinated at residual risk.
Ryan Hlavaty
October 17, 2025 AT 22:23It is indefensible to ignore these data; one should prioritize evidence‑based interventions and not rely solely on a presumed 60 % protection claim.
Chris Faber
October 18, 2025 AT 17:50Cool info, thanks for breaking it down!
aura green
October 19, 2025 AT 13:17Wow, look at this epic guide – it’s basically the “choose your own adventure” of flu misery.
First, you get a fever, which is the universe’s way of saying “hey, you’re alive!”.
Then you might develop a cough that sounds like a dying cat, because why not add drama?
Next up, the dreaded pneumonia, the grand finale that makes you wonder if you’ll ever breathe again.
If you’re lucky, you’ll also get sinusitis, which is basically a party in your nose that nobody invited.
And don’t forget the classic ear infection, because who doesn’t love a ringing soundtrack?
For the really brave, there’s myocarditis – your heart decides to join the party and goes all “beat‑beat‑beat”.
If you’re into brain games, encephalitis will give you a very literal brain fog.
All of this, while you’re trying to stay hydrated, but the flu steals your water like a sneaky thief.
Good news: vaccination can cut the drama by up to 60 %, which is like getting a 40 % discount on a nightmare.
Even better, antivirals work if you start them within 48 hours – they’re the flash‑sale of flu treatment.
Don’t forget to wash your hands; soap is the unsung hero of the pandemic world.
And if you’re at high risk, the doctor might give you a high‑dose shot, which feels like a superhero cape.
Bottom line: treat the flu like an unwanted houseguest – give it a short stay and kick it out fast.
Stay safe, stay hydrated, and for the love of everything, get your flu shot. 😜
Sriram K
October 20, 2025 AT 08:43Appreciate the comprehensive layout. For anyone juggling diabetes, keep glucose monitoring tight – flu can spike blood sugar unexpectedly. Also, coordinate with your primary care provider about prophylactic antivirals if you fall into a high‑risk category.
Deborah Summerfelt
October 21, 2025 AT 04:10If we accept the premise that flu is merely a seasonal inconvenience, then the entire preventive paradigm collapses into a self‑fulfilling prophecy, rendering vaccination a symbolic gesture at best.
Maud Pauwels
October 21, 2025 AT 23:37Thank you for the clear summary.
Scott Richardson
October 22, 2025 AT 19:03Our country needs to invest more in vaccine research, period.
Laurie Princiotto
October 23, 2025 AT 14:30Stop wasting time, get vaccinated already! 😡
Justin Atkins
October 24, 2025 AT 09:57From a virological standpoint, the antigenic shift inherent to influenza viruses necessitates an annual immunization strategy. Empirical data indicate that even a modest reduction in viral load can substantially lower the incidence of secondary bacterial pneumonia. Moreover, the pharmacokinetics of oseltamivir suggest optimal efficacy when administered within the first 48 hours of symptom onset, underscoring the importance of early medical consultation. In tandem, public health policies should prioritize outreach to high‑risk cohorts-namely, the geriatric population, pregnant individuals, and those with chronic comorbidities-to ameliorate morbidity metrics.
June Wx
October 25, 2025 AT 05:23Yeah, whatever, just do it already.