When you feel a sharp, steady pain under your right rib cage that lasts for hours and doesn’t go away with gas or vomiting, it’s not just indigestion. It could be gallstones - and if this happens more than once, it’s time to pay attention. About 1 in 10 adults in developed countries has gallstones, but most never know it. The real problem starts when those stones block the flow of bile. That’s when biliary colic turns into cholecystitis, and surgery stops being an option - and becomes a necessity.
What Exactly Is Biliary Colic?
Biliary colic isn’t an infection. It’s a warning sign. It happens when a gallstone gets stuck in the cystic duct - the tube that drains bile from your gallbladder. The muscle in the gallbladder contracts hard trying to push bile through, but the stone blocks it. That’s when the pain hits.
The pain is intense, localized to the upper right side of your abdomen or just below your breastbone. It doesn’t come in waves like cramps. It’s steady, builds up within an hour, and lasts 1 to 5 hours. You can’t relieve it by moving, burping, or having a bowel movement. Many people mistake it for heartburn or a stomach bug. But if you’ve had it once, there’s a 90% chance you’ll have it again within 10 years. Two-thirds will get it back within two years.
Most gallstones are made of cholesterol - about 80% in Western countries. The rest are pigment stones, formed from excess bilirubin. They don’t form because of diet alone. It’s about how your body processes bile. If your gallbladder doesn’t empty often enough, cholesterol crystals build up. Obesity, rapid weight loss, pregnancy, and certain medications all raise your risk.
When Biliary Colic Turns Into Cholecystitis
If the stone stays stuck for more than a few hours, your gallbladder starts to swell and get inflamed. That’s acute cholecystitis. It’s no longer just pain - it’s infection waiting to happen.
Symptoms get worse: fever, nausea, vomiting, and tenderness when you press on your right side. The pain doesn’t fade - it lingers for days. Blood tests show elevated white blood cells and liver enzymes. An ultrasound will reveal a thickened gallbladder wall and maybe even fluid around it.
One in five people who have biliary colic will develop cholecystitis. And if left untreated, it can lead to a ruptured gallbladder, sepsis, or stones moving into the common bile duct - causing jaundice or pancreatitis. The NHS reports that 20-30% of people with untreated symptomatic gallstones end up in the emergency room within five years.
That’s why timing matters. The Society of American Gastrointestinal and Endoscopic Surgeons says cholecystectomy should happen within 72 hours of diagnosing acute cholecystitis. Waiting longer increases the chance your surgery will need to be done the old-fashioned way - with a large incision - instead of the minimally invasive option.
Why Laparoscopic Cholecystectomy Is the Gold Standard
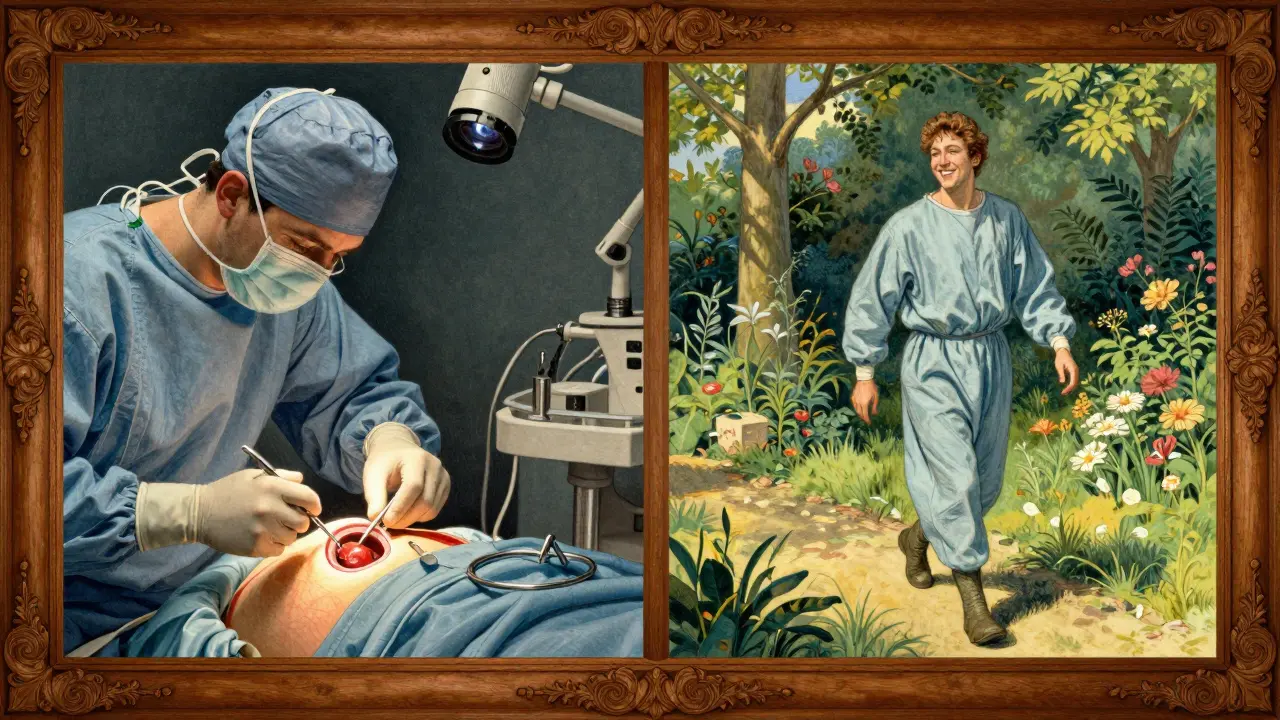
For most people with recurring gallstone symptoms, removing the gallbladder is the only reliable fix. And the standard procedure today is laparoscopic cholecystectomy.
This isn’t open surgery with a big cut. It’s done through four tiny incisions. A camera and thin instruments go in, the gallbladder is carefully detached, and removed. The average operation takes 45 to 60 minutes. Most patients go home the same day or the next morning.
Compared to open surgery, recovery is dramatically faster: 7 days versus 30. Hospital stays drop from nearly 5 days to just over 1. Pain is much less. Scarring is minimal. And success rates? Around 95% of patients report major improvement in quality of life.
It’s not without risks. About 5-10% of cases need to be switched to open surgery because of severe scarring, anatomy problems, or uncontrolled bleeding. But in experienced hands, serious complications - like bile duct injury - happen in less than 2% of cases.
Patients under 75 with no major health issues have a 30-day mortality rate below 0.1%. That number jumps to 2.8% for those over 75 with three or more chronic conditions. That’s why doctors don’t rush surgery for frail elderly patients unless absolutely necessary.
What About Non-Surgical Options?
Some people hear "surgery" and panic. They look for alternatives. There are options - but they’re not replacements.
Ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones. But it only works in 30-50% of cases, and it takes 6 to 24 months. Even if it works, half the stones come back within five years. It’s mostly used for people who can’t have surgery - not as a first choice.
Shock-wave lithotripsy breaks stones apart with sound waves, then uses medication to dissolve the fragments. It had promise in the 90s, but recurrence rates were too high. Today, it’s rarely used.
Endoscopic ultrasound-guided drainage is new. The FDA approved it in 2023. It’s for high-risk patients who can’t tolerate surgery. A tiny tube is placed into the gallbladder to drain it, buying time. It’s not a cure - it’s a bridge. One study showed 85% success in stabilizing patients who were too sick for surgery.
There’s no magic pill. Diet changes won’t make gallstones disappear. Low-fat diets help reduce attacks, but they don’t stop stones from forming. Supplements, herbal remedies, and gallbladder flushes? No scientific backing. Don’t waste time or money on them.
What Happens After Surgery?
People worry about living without a gallbladder. The truth? Most don’t notice a difference.
The liver still makes bile. Without the gallbladder to store it, bile flows directly into the small intestine. Some people get looser stools for a few weeks - especially after fatty meals. That usually settles down. About 12% report ongoing diarrhea. A small number - around 6% - develop post-cholecystectomy syndrome: persistent pain, bloating, or nausea. That’s often because something else is wrong - like bile duct stones, Sphincter of Oddi dysfunction, or even undiagnosed IBS.
Recovery is quick. Most get up and walk within 4 hours. Start sipping water and clear liquids within 6 hours. Solid food by the next day. Return to light work in a week. Heavy lifting? Wait 4 to 6 weeks.
One patient from Cleveland Clinic had 17 episodes of biliary colic over 18 months. After surgery, her pain vanished. Within 10 days, she was back to hiking. Two weeks later, she was back at work. That’s the norm, not the exception.

Who Should Consider Surgery - And Who Should Wait?
Not everyone with gallstones needs surgery. But if you’ve had biliary colic, and you’re under 75 with no major heart or lung disease, the answer is almost always yes.
Here’s the rule of thumb:
- Have had one or more attacks? → Surgery is strongly recommended.
- Have diabetes or heart disease? → Talk to your doctor. Risk is higher, but so is the danger of waiting.
- Over 75 with multiple chronic illnesses? → Conservative management may be safer. Monitor closely.
- Have stones but zero symptoms? → Leave them alone. Only 1-3% develop symptoms each year.
Women are 2 to 3 times more likely to get gallstones than men. Hispanic populations have a 45% higher risk than non-Hispanic whites. Obesity is the biggest driver. The global market for gallstone treatments is growing - not because more people are getting sick, but because more people are getting diagnosed and treated.
What Patients Say - Real Stories
A Healthline survey of over 1,200 people found that 78% chose surgery after three or more episodes. Sixty-five percent said severe pain that sent them to the ER was the deciding factor.
On Reddit, 82% of those who had laparoscopic surgery said their quality of life improved within two weeks. The complaints? Diagnostic delays - 41% saw three or more doctors before getting an ultrasound. And 29% said their pain wasn’t managed well during the attack. That’s the hidden problem: doctors miss it. Pain is dismissed as indigestion. Ultrasounds aren’t ordered fast enough.
One man in his 50s waited six months because his GP said it was "just gas." He ended up in the ER with cholecystitis. His surgery was delayed. He needed an open procedure. Recovery took two months. He told his story to warn others: "If your pain is sharp, steady, and doesn’t go away - get an ultrasound. Don’t wait."
Can gallstones go away on their own?
No. Once gallstones form, they don’t dissolve on their own. Some people never have symptoms, so they live with them. But if they cause pain or inflammation, they won’t disappear without treatment. Medications like ursodeoxycholic acid can dissolve small cholesterol stones in some cases, but this takes months and has a high recurrence rate. Surgery remains the only permanent solution.
Is laparoscopic surgery better than open surgery for gallstones?
Yes, for most people. Laparoscopic cholecystectomy uses small incisions, has less pain, shorter hospital stays (1-2 days vs. 4-7 days), and faster recovery (1 week vs. 4-6 weeks). It’s the standard today, used in over 90% of cases in the U.S. Open surgery is only needed if there’s severe inflammation, scarring, or complications during the laparoscopic procedure.
What are the risks of gallbladder removal?
Serious complications are rare - under 2% in experienced hands. The most common risks include bleeding, infection, and injury to the bile duct (which happens in less than 1% of cases). Some people have looser stools after surgery, especially after fatty meals, but this usually improves over time. A small number develop post-cholecystectomy syndrome, which may require further testing to rule out other issues like bile duct stones or IBS.
Can I prevent gallstones with diet?
Diet alone can’t prevent gallstones, but it can reduce the chance of attacks. Avoiding rapid weight loss, eating regular meals, and limiting high-fat, high-sugar foods helps. Obesity and diabetes are major risk factors, so maintaining a healthy weight and managing blood sugar are key. No specific food causes gallstones, but skipping meals or crash dieting increases risk.
Why do some people still have pain after gallbladder removal?
Pain after surgery doesn’t always mean the operation failed. About 6-12% of people report ongoing symptoms. This could be due to bile duct stones that weren’t removed, Sphincter of Oddi dysfunction, irritable bowel syndrome, or even acid reflux. In rare cases, a stone may have been left behind. If pain persists, further tests - like an MRI of the bile ducts or an endoscopic ultrasound - are needed to find the real cause.
When you’re in pain, waiting for answers is the hardest part. But once you have a diagnosis, the path forward is clear. Gallstones aren’t a mystery anymore. We know what causes them. We know how to treat them. And for most people, the solution is simple: remove the source. Not because it’s drastic - but because it works.


PAUL MCQUEEN
February 7, 2026 AT 19:49Ugh, I swear every time I go to the doctor with abdominal pain they just hand me Tums and call it a day. Had two episodes last year - thought it was food poisoning. Turns out? Gallstones. Took six weeks to get an ultrasound. By then, I was in cholecystitis mode. Surgery was a breeze, but the system? Total joke.
Don’t wait like I did. If it’s steady pain under the ribs? Get scanned. No excuses.
Chima Ifeanyi
February 8, 2026 AT 09:55Let’s deconstruct this narrative through a political economy lens: the commodification of cholecystectomy as a ‘gold standard’ is a direct product of neoliberal healthcare incentivization. The laparoscopic procedure isn’t superior - it’s profitable. Hospitals push it because reimbursement rates are higher, and insurers favor shorter stays.
Meanwhile, in Nigeria, where ultrasound access is scarce and surgical capacity is strained, conservative management remains the pragmatic default. This isn’t medical wisdom - it’s capital logic dressed in white coats.
Tatiana Barbosa
February 9, 2026 AT 21:25Y’all need to hear this: if you’ve had one biliary colic episode, DO NOT WAIT. I had mine at 29 - thought I was just stressed. My GP said ‘maybe acid reflux.’ Two months later, I was in the ER with fever and a swollen gallbladder. They had to do open surgery because I waited.
Now I’m 31, no gallbladder, hiking every weekend. I wish I’d listened to my gut - literally. Your body screams before it breaks. Listen.
And no, kale smoothies won’t fix it. 😘
MANI V
February 11, 2026 AT 06:14Look, I get it - you want a quick fix. But let’s be real: gallbladder removal is just a Band-Aid on a systemic failure. Your liver’s still making bile, but now it’s dumping it like a drunk guy at a party - no regulation, no storage, no dignity.
And don’t even get me started on the ‘95% success rate.’ That’s marketing. What about the 5% who end up with bile reflux, chronic diarrhea, or Sphincter of Oddi dysfunction? Nobody talks about that.
You’re not cured. You’re just… redirected.
Susan Kwan
February 11, 2026 AT 07:41So let me get this straight - you’re telling me the solution to a 90% recurrence rate is to cut out the whole organ?
And nobody’s asking why this is happening in the first place? No one’s talking about the fact that we’re eating like robots, moving like zombies, and our bodies are just… giving up?
It’s not the gallbladder that’s broken. It’s the whole damn system.
Ryan Vargas
February 13, 2026 AT 04:17Consider the metaphysical implications of gallstone formation: the body, as a self-regulating organism, does not produce pathological crystallization without a deeper signal. The gallbladder, a reservoir of bile, is not a passive container - it is a dynamic organ of metabolic intentionality.
When cholesterol precipitates, it is not merely a biochemical anomaly - it is a somatic protest against chronic metabolic neglect: sedentary life, emotional suppression, circadian disruption, and the industrialization of digestion.
Removal is a surgical capitulation. The real question is not whether to operate - but why the body felt compelled to build this fortress of stone in the first place.
Tasha Lake
February 14, 2026 AT 14:42Wait - so UDCA works in 30-50% of cases but takes 6–24 months? And half recur? That’s wild.
So if I’m under 75, no comorbidities, and had one attack - surgery is the move. But if I’m over 75 with three chronic illnesses? Maybe don’t.
What about someone in their 60s with one chronic condition? Where’s the line? This feels like a gray zone they gloss over.
Also - is there data on how many people *regret* surgery? Like, ‘I wish I’d tried the meds’? Just curious.
Simon Critchley
February 15, 2026 AT 09:15LOL at the ‘gallbladder flush’ crowd. You’re not ‘detoxing’ with olive oil and lemon juice - you’re just giving yourself diarrhea while feeling like a wellness influencer.
I had mine out in 2019. Four incisions. Home by noon. Back to gaming by day 3. No more ‘oh no, I can’t eat pizza’ nonsense.
My ex still swears by ‘herbs’ and won’t get scanned. She’s now on 24/7 antacids. I just laugh. She’s got a stone the size of a marble. And a lifetime of regret. 😎
Tom Forwood
February 17, 2026 AT 00:19Yo, I’m from Texas - we don’t mess around with gallstones here. My cousin had four attacks in a year. Went to three docs. First said ‘stress.’ Second said ‘lactose.’ Third said ‘maybe wait.’
Finally, his wife made him go to a GI specialist. Ultrasound showed three stones. Surgery next week.
Now he’s back to grilling brisket like nothing. No pain. No regrets. Just one less organ and a whole lot more freedom.
Don’t be like my cousin. Get it checked. Seriously. It’s not a ‘maybe.’
John McDonald
February 17, 2026 AT 04:47So many people don’t realize this: gallstones aren’t rare. They’re just silent until they’re not.
I had zero symptoms for years. Then one day - boom. 5 hours of pain, sweating, nausea. Thought I was dying. Turned out my gallbladder looked like a rock garden.
After surgery? Life changed. I could eat cheese again. I could sleep. I could breathe.
Don’t wait for it to get ugly. If you’ve had one episode? You’re already on the path. Just move.
Jacob den Hollander
February 17, 2026 AT 11:19Just wanna say - I’m so glad I found this. My mom had gallstones and they didn’t do anything for months because she was ‘too old.’ She ended up in the hospital with sepsis. We were lucky she made it.
Now I’m 34, and I get checked every year. I eat regular meals. I don’t skip breakfast. I walk every day.
It’s not glamorous. But it’s better than waiting for your body to break.
Thank you for writing this. Really. I’m sharing it with everyone I know.
Andrew Jackson
February 17, 2026 AT 19:10It is an affront to Western medical ethics that we have allowed the gallbladder - a vital organ of digestion and bile regulation - to be routinely excised as if it were a benign tumor.
Compare this to the surgical removal of the appendix: a vestigial organ. The gallbladder, however, is not vestigial. It is a sophisticated reservoir, an organ of metabolic precision, and its removal constitutes a form of biological reductionism.
One must ask: why are we so quick to cut? Why not restore? Why not heal? The answer lies not in medicine, but in profit.
It is a tragedy. And a betrayal of the human body.
Camille Hall
February 18, 2026 AT 00:24My sister had her gallbladder out last year. She was terrified. But now? She says it’s like a weight lifted. She didn’t even know how much pain she was living with until it was gone.
And honestly? The recovery was easier than her C-section. Who knew? I thought surgery meant weeks of agony.
She’s back to yoga, cooking, traveling - all the things she loved. Just no more panic attacks before meals.
If you’re thinking about it - do it. You’ll thank yourself.
Ritteka Goyal
February 18, 2026 AT 22:08Bro I had gallstones too in 2022 and I did not go to doctor because I thought it was just spicy food 😅 I ate 3 plates of biryani and then boom - 12 hours of pain. My mom dragged me to hospital. They said I was lucky it didn’t rupture.
Now I eat less oil, more oats, and I drink warm water in morning. No more attacks.
But surgery? I think if you can manage with diet, why cut? Maybe I’m just lucky.
Also I’m from India - we don’t do surgery for everything like USA 😅