Every year, 100 million people are pushed into extreme poverty because they can’t afford medicine. In many low-income countries, a single course of antibiotics or antiretroviral drugs can cost more than a week’s wages. Yet the solution isn’t hidden in some high-tech lab-it’s already sitting on pharmacy shelves in the form of generic drugs. These are the same medicines as the branded ones, just without the patent, the marketing, and the price tag. For millions, they’re the only thing standing between life and death.
What Exactly Are Generics?
Generics are drugs that contain the exact same active ingredients as brand-name medicines. They work the same way, in the same dose, with the same safety profile. The only differences? They’re not branded, they don’t come with flashy packaging, and they cost up to 80% less. In the U.S., 9 out of 10 prescriptions are filled with generics. In low-income countries? Only about 5% of medicines sold are unbranded generics. That’s not because they’re less effective-it’s because the system is broken.Why Aren’t Generics More Widely Used?
It’s not a lack of supply. Companies like Cipla, Hikma, and Sun Pharma make billions of doses of generic HIV, malaria, and tuberculosis drugs every year. The problem isn’t that they don’t exist-it’s that they don’t reach the people who need them most. Many governments still charge high import taxes and tariffs on generic drugs. In some African countries, a simple malaria treatment that costs $0.10 to produce ends up costing $3 by the time it hits a rural clinic because of customs fees, middlemen, and poor logistics. Even when drugs arrive, clinics often don’t have refrigerators to store them, or staff to manage inventory. Out of stock? That’s the norm, not the exception. Then there’s the trust issue. Patients and even doctors in some regions are afraid generics are fake or weak. That fear isn’t completely unfounded-counterfeit drugs are a real problem in places with weak regulation. But the real issue? Most of the generics that do reach patients are quality-assured, yet they’re still ignored because of stigma. People pay more for a branded pill because they believe it’s safer-even if it’s the exact same medicine.How Much Do Generics Actually Save?
The numbers speak for themselves. A course of generic antiretroviral therapy for HIV used to cost over $10,000 a year in the early 2000s. Today, thanks to generics, it’s under $75. That’s not a small drop-it’s a revolution. In countries like South Africa and Kenya, this price collapse allowed national health programs to treat millions who were previously locked out. The same story played out with tuberculosis drugs and artemisinin-based malaria treatments. When prices fell, treatment rates soared. The World Health Organization estimates that without generics, global efforts to control HIV and malaria would have failed. Yet even now, over 2 billion people still can’t access the essential medicines they need. Why? Because savings don’t automatically mean access.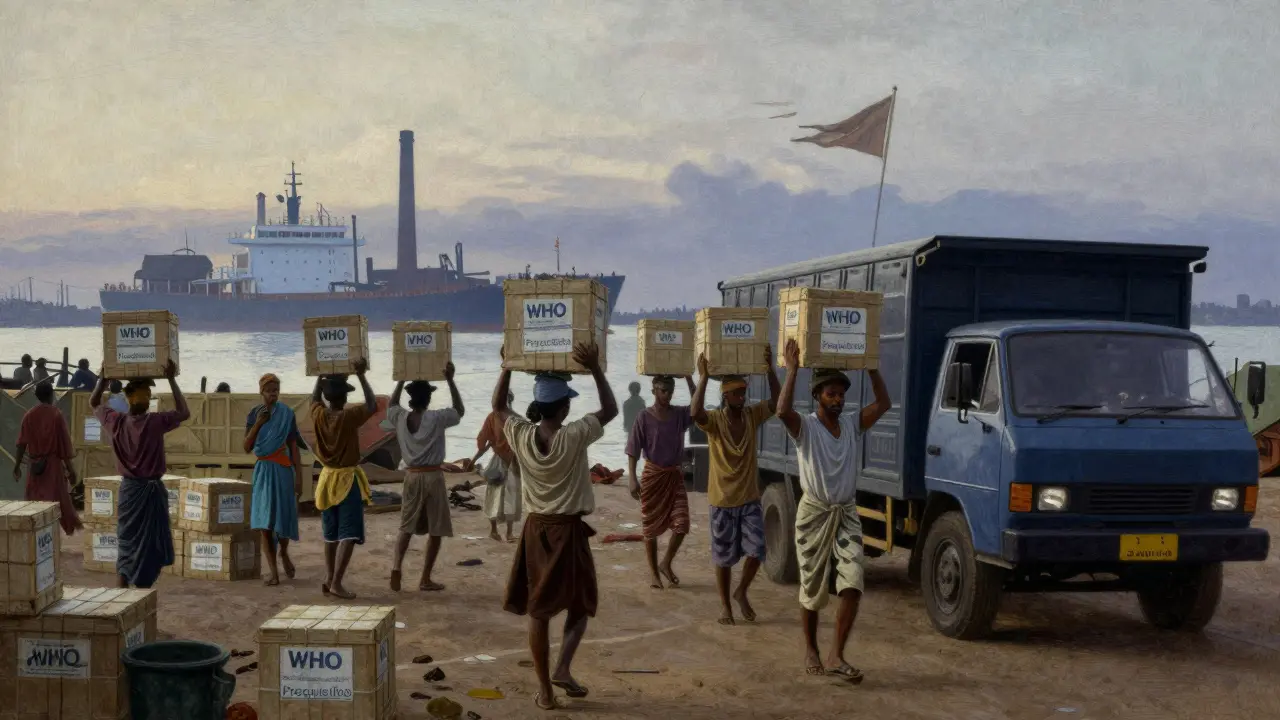
The Broken Supply Chain
You can have the cheapest medicine in the world, but if it never reaches the clinic, it doesn’t help anyone. In many low-income countries, the supply chain is fragile. Roads are bad. Power outages kill refrigerated drugs. Health workers aren’t trained to track inventory. A study in the Lancet found that public clinics in the Western Pacific region saw medicine availability drop by over 5% in the last decade-even as global production of generics rose. Compare that to Europe, where public investment and strong logistics systems pushed medicine availability up by nearly 28% in public clinics since 2009. The difference isn’t technology-it’s commitment. Countries that treat medicine access like a public service, not a commodity, get results.Who’s Making This Work?
Some companies are trying. The Access to Medicine Foundation tracked five major generic manufacturers-Cipla, Hikma, Sun Pharma, Teva, and Viatris-and found they cover 90% of the essential off-patent drugs needed in low-income countries. But here’s the catch: only 41 of those 102 drugs had any real strategy to make them affordable for the poorest patients. Most focused on selling to governments or big NGOs, not on reaching people who pay out of pocket. Meanwhile, big pharma companies like Novartis and Pfizer have their own access programs. They offer discounted drugs or donate supplies. But they rarely publish data on how many people actually get those medicines. Transparency is missing. You can’t fix a problem you won’t measure.What Needs to Change?
There are five clear, practical steps that would make a massive difference:- Remove taxes and tariffs on essential generic medicines. A 10% import tax on a $0.20 malaria drug adds $0.02-but that $0.02 can mean the difference between treatment and death in a household living on $2 a day.
- Simplify drug approval. In some countries, it takes over two years to approve a generic drug. In others, like India and South Africa, the process takes under six months. Why? Because they prioritized speed over bureaucracy.
- Invest in public health systems. The African Union promised in 2001 to spend at least 15% of national budgets on health. As of 2022, only 23 of 54 African countries met that target. Without funding, clinics stay empty, even if drugs are available.
- Build local manufacturing. Countries like India and Bangladesh produce most of the world’s generics. But most low-income countries don’t make any. Building local capacity reduces dependency on imports and creates jobs.
- Use data to track supply. Seventy-six percent of healthcare organizations in emerging markets are now investing in big data to monitor drug availability. That’s progress. But data only matters if it leads to action.

Real Stories, Real Impact
In Uganda, a woman named Amina was diagnosed with HIV in 2018. She lived in a village three hours from the nearest clinic. Before generics, her monthly treatment would have cost her family’s entire income. Instead, thanks to a government program using generic antiretrovirals, she pays nothing. Her viral load is undetectable. Her children are healthy. She works as a community health volunteer now, helping others get tested. That’s not a miracle. That’s policy. That’s generics working as they should.Why This Matters Beyond Health
Access to medicine isn’t just a health issue-it’s an economic one. When people can’t afford treatment, they drop out of school, lose jobs, and fall deeper into poverty. Families sell land, take out loans, or pull children out of school to pay for medicine. That’s why 100 million people are pushed into extreme poverty every year. Generics break that cycle. They don’t just save lives-they preserve livelihoods. They let parents work, children learn, and communities thrive.The Road Ahead
The tools to fix global health access already exist. We know how to make cheap, effective medicines. We know how to deliver them. We know what policies work. What’s missing is political will. Countries that treat medicine as a right, not a luxury, see results. The U.S. uses generics because it has strong regulation and public trust. Europe uses them because it invests in public health. India and Bangladesh use them because they built their own manufacturing. The rest can too. The next time you hear someone say, "We can’t afford to treat everyone," remember: we already can. We just haven’t chosen to.Are generic drugs safe in low-income countries?
Yes, if they’re quality-assured. Many generic drugs used in low-income countries are manufactured under strict standards by companies approved by the World Health Organization or other international regulators. The problem isn’t safety-it’s supply, regulation, and misinformation. Counterfeit drugs are a real threat, but they’re not the same as legitimate generics. Always check for WHO prequalification or other certification on packaging.
Why don’t governments just buy more generics?
Many do-but they’re often blocked by bureaucracy, corruption, or lack of funding. Some governments still prefer branded drugs because they’re easier to track or because they’ve been pressured by pharmaceutical companies. Others simply don’t have the budget to stock enough medicines, even if they’re cheap. The real issue isn’t cost-it’s political priority.
Do generic drugs work as well as branded ones?
Yes. By law, generics must contain the same active ingredient, in the same strength, and work the same way in the body. They go through the same testing for safety and effectiveness. The only differences are in inactive ingredients, packaging, and price. In the U.S., 90% of prescriptions are generics-and they’re trusted by doctors and patients. There’s no scientific reason to believe they’re less effective.
Why do people in low-income countries still pay out of pocket?
Because most low-income countries have no universal health coverage. Over 90% of people in these nations pay for medicine themselves. Even when drugs are available, clinics often require cash payment upfront. Without insurance or government subsidies, families are forced to choose between medicine and food. That’s why eliminating out-of-pocket payments is one of the most urgent steps needed.
Can low-income countries make their own generics?
Yes, and some already do. India and Bangladesh are global leaders in generic drug production. Countries like Kenya, Nigeria, and Ethiopia are building local capacity too. But it takes investment in factories, training, and regulation. International support helps, but the real driver is local political will. When governments prioritize domestic production, they reduce dependency and lower costs.
What role do patents play in limiting access?
Patents give companies exclusive rights to sell a drug for 20 years, preventing generics from entering the market. But international rules allow low-income countries to ignore patents for public health emergencies-like HIV or malaria. The problem? Many countries don’t know how to use these flexibilities, or they’re pressured by wealthy nations and drug companies not to. The TRIPS Agreement lets them act-but political pressure often stops them.
How can I help improve access to generics?
Support organizations that advocate for fair drug pricing and transparent supply chains. Donate to groups that deliver quality-assured generics to clinics. Push your government to fund global health initiatives. And don’t believe the myth that generics are inferior-demand better policies, not more expensive drugs.


Edith Brederode
January 19, 2026 AT 14:17This made me cry. Seriously. I had no idea generics could save so many lives for pennies. 🥺 My grandma took generics for her blood pressure for 20 years-same pills, 1/10th the cost. Why do we make this so complicated?
clifford hoang
January 20, 2026 AT 23:09Generics? LOL. You think Big Pharma doesn’t control the WHO and the FDA? 🤔 The real story? They let generics in *just enough* to look good while quietly lobbying to keep the real cures locked behind patents. They’re not saving lives-they’re managing PR. Wake up. The system is rigged. 🧠💊
Arlene Mathison
January 21, 2026 AT 09:52YES. This is the kind of change we can actually *do* something about. Not some sci-fi tech solution-just *using what already works*. I’m so tired of people waiting for miracles when the answer is right in front of us. Let’s fund clinics. Let’s cut taxes. Let’s stop pretending poor people don’t deserve the same meds we get. 💪🌍
Emily Leigh
January 23, 2026 AT 02:49Okay but… are we *sure* generics aren’t just… cheaper because they’re worse? I mean, I’ve seen knockoff sunglasses that look like Gucci but fall apart in the rain. Same thing here? 🤨 Also, why is everyone acting like this is new? I read this exact thing in 2012. Nothing changed. Nothing ever does.
Carolyn Rose Meszaros
January 23, 2026 AT 08:54That story about Amina? I’m saving this. 🫶 I’m sharing it with my book club. Also-can we talk about how wild it is that we treat medicine like a luxury item? Like, we have the tech, the science, the supply… we just don’t care enough. 😔
Greg Robertson
January 24, 2026 AT 04:19Really well written. I’m a nurse in rural Ohio-we use generics every day. Patients love them. They’re safe, they work, and they don’t break the bank. It’s frustrating when people think branded = better. It’s not. Just… trust the science. 😊
Renee Stringer
January 26, 2026 AT 00:58It’s not about access-it’s about responsibility. If people can’t afford medicine, maybe they shouldn’t be getting sick in the first place. Poor choices lead to poor outcomes. Why should taxpayers fund the consequences of bad lifestyle decisions? 🙄
Courtney Carra
January 26, 2026 AT 22:10Think about it: the same molecules, the same chemistry, the same biological pathways. The only variable is the label. If you believe in the sanctity of the human body, then you must believe that a molecule doesn’t care if it’s in a $100 bottle or a $1 bottle. The system isn’t broken-it’s morally bankrupt.
thomas wall
January 28, 2026 AT 10:52It is profoundly disturbing that in the 21st century, a child in Malawi must die because a pharmaceutical conglomerate holds a patent on a compound synthesized in 1978. This is not healthcare. This is colonialism with a prescription pad. The world has failed. And we-those of us who live in comfort-have chosen to look away.
Manoj Kumar Billigunta
January 29, 2026 AT 20:51As someone from India, I’ve seen this up close. Cipla made HIV meds for $1 a day in 2001. The world called it a miracle. But now? We’re still waiting for the rest of the world to catch up. It’s not about technology. It’s about justice. We can do this. We’ve done it before. Let’s not forget how.
Thomas Varner
January 31, 2026 AT 04:07Wait-so you’re saying we just need to… remove taxes? And fix supply chains? And stop being racist against cheap medicine? That’s it? No AI? No blockchain? No $50M startup? 😅