Protein-Levodopa Interaction Calculator
Enter your protein intake for each meal to see how it aligns with the Protein Redistribution Diet (PRD) recommendations. Keep daytime meals under 7g of protein to maximize levodopa effectiveness.
For optimal levodopa effectiveness:
- Breakfast and lunch: Under 7g protein
- Dinner: Up to 30g protein
If you or someone you know takes levodopa for Parkinson’s disease, eating a steak, chicken breast, or even a big bowl of beans might be making symptoms worse-without you even realizing it. It’s not about bad food. It’s about biology. The same amino acids that build muscle also block the medicine meant to restore movement. This isn’t a myth or a guess. It’s been studied for decades, and the science is clear: protein and levodopa compete for the same doorway into your brain.
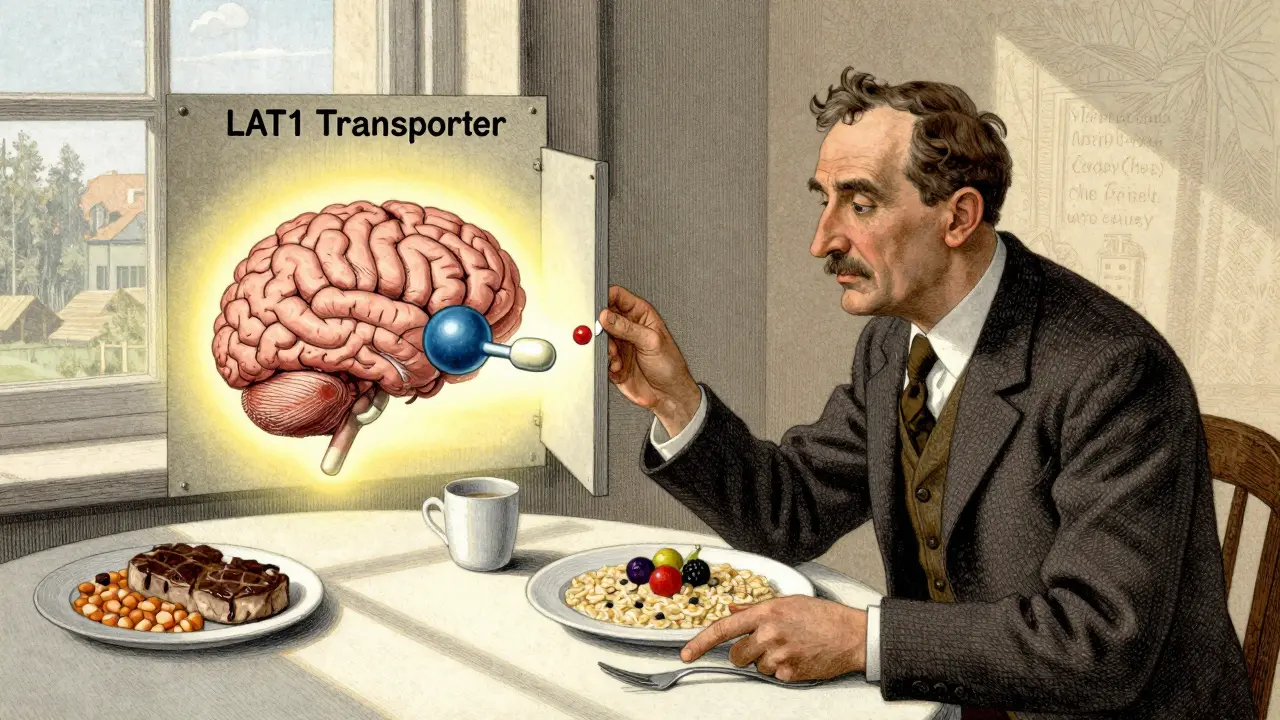
Why Protein Blocks Levodopa
Levodopa doesn’t just float into your brain after you swallow it. It needs a special transport system called LAT1 to cross the blood-brain barrier. This system is designed to carry large neutral amino acids (LNAAs)-like leucine, phenylalanine, and tryptophan-into the brain because they’re essential for making neurotransmitters. But here’s the problem: levodopa looks just like these amino acids. So when you eat a high-protein meal, your blood fills up with these competing molecules. They crowd the transporter. Levodopa gets pushed to the back of the line. Studies show that after a meal with 20 grams or more of protein, levodopa absorption drops by 25-40%. Its peak level in the blood is delayed by 45 to 90 minutes. That delay doesn’t just mean your pill takes longer to work-it means you might be stuck in an "off" period when your body feels frozen, shaky, or unresponsive, even though you took your medicine on time. This isn’t a problem everyone has. About 40-50% of people on long-term levodopa develop this issue. It usually shows up 8-13 years after starting treatment, often when motor fluctuations become more frequent. If you’re noticing your meds work great in the morning but fail after lunch, protein is likely the culprit.The Three Ways People Manage This
There are three main dietary strategies doctors recommend to reduce this interference. None are perfect. But one stands out.- Low-Protein Diet (LPD): This cuts total daily protein to 40-50 grams-roughly half of what most adults eat. A 60kg person might eat two eggs (12g), a small fish fillet (20g), and half a cup of lentils (8g). It sounds simple, but it’s hard to sustain. Many people lose weight, get weak, or feel exhausted because they’re not getting enough protein for muscle and immune health.
- Protein Redistribution Diet (PRD): This is the most effective method. You eat almost all your protein in the evening-after your last levodopa dose-and keep daytime meals low in protein (under 7g per meal). That means breakfast and lunch might be rice, fruit, vegetables, and bread. Dinner is your steak, tofu, or beans. Research shows PRD reduces "off" time by nearly two hours a day and adds 30 minutes of smooth, controlled movement. It works best for people in Hoehn & Yahr stages 3 or 4, where motor fluctuations are most disruptive.
- Low-Protein Products (LPP): These are specialty foods-protein-free pasta, bread, and flour-made to help people stick to low-protein meals. They help, but only a little. Only 22% of users say they feel more satisfied with their diet using them. They’re expensive and hard to find outside big cities.
Why PRD Works Better Than Cutting Protein Altogether
You might think, "If protein interferes, why not just eat less of it?" But the body needs protein. Not just for muscles, but for healing, immunity, and hormone balance. A strict low-protein diet can lead to muscle loss, slower recovery from illness, and even malnutrition. In one study, 31% of people on LPD lost more than 5% of their body weight in six months. PRD avoids this. You still get your full daily protein-just at a time when it won’t interfere. Levodopa is absorbed best in the morning and early afternoon, when most people are active. By saving protein for the evening, you let your medicine work when you need it most. And at night, when you’re less active, even if levodopa absorption is slowed, it doesn’t matter as much. A 2017 study found PRD reduced motor fluctuations by 35% more than standard low-protein diets. People on PRD reported fewer sudden freezes, better walking, and more control over tremors during the day. It’s not magic-but it’s the most reliable tool we have.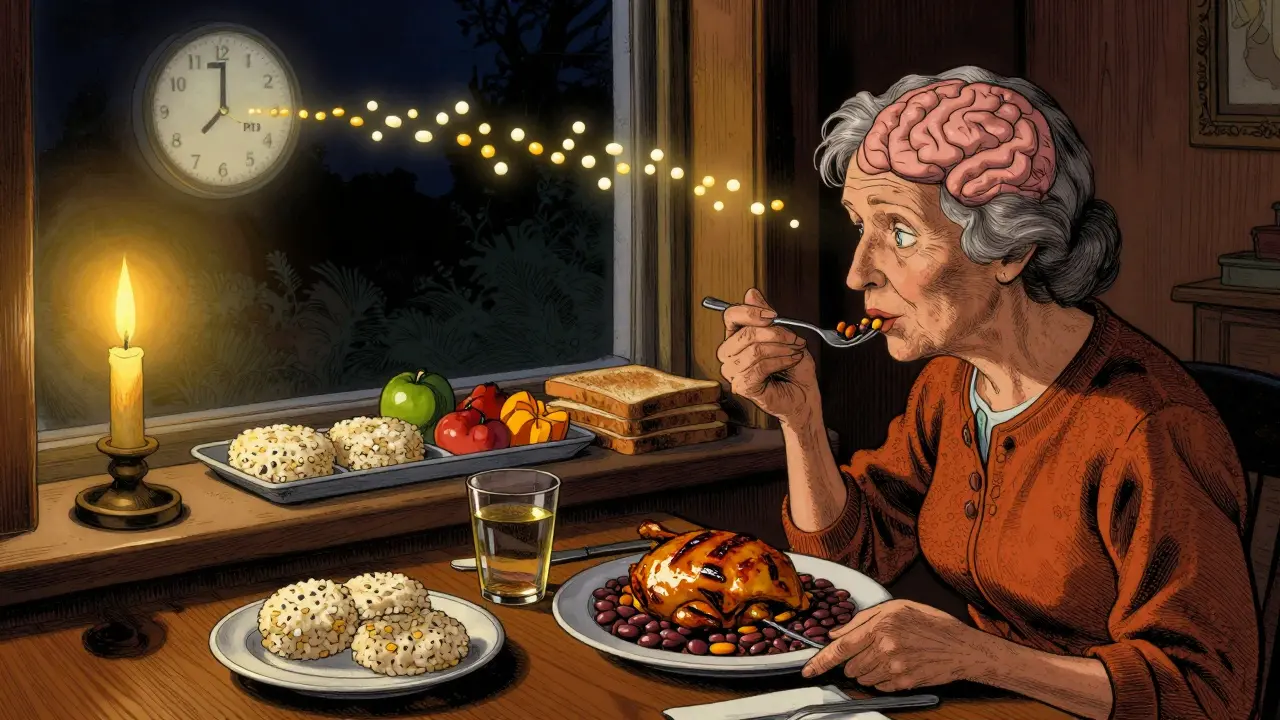
What Doesn’t Work (And Why)
Some people try timing their pills 30-60 minutes before meals. It sounds logical. But it’s inconsistent. If your stomach is slow, or you have gastroparesis (common in Parkinson’s), the pill might sit there for hours before being absorbed. You could end up taking it too early and still having protein compete with it later. Another myth: "Just eat protein with your pill to balance it out." That’s not how it works. The competition happens in your bloodstream and at the blood-brain barrier. It doesn’t matter if they’re in your stomach together. The amino acids still flood the transporters and block levodopa. And no, protein supplements or shakes won’t help unless they’re specifically designed as low-protein. Most protein powders contain 20-30 grams of amino acids per serving-enough to shut down levodopa absorption completely.Real People, Real Struggles
It’s not just science. It’s life. One Reddit user, u/ParkinsonsWarrior, said after switching to PRD under dietitian guidance, he gained 2.5 extra hours of reliable mobility each day. That’s not just comfort-it’s independence. He could walk to the mailbox, carry groceries, and play with his grandkids without fear of freezing mid-step. But many others quit. A 2023 review found 68% of people stopped PRD within a year. Why? Social isolation. Family dinners become awkward. Holidays feel like a minefield. A 58% of users reported avoiding gatherings because they couldn’t eat what everyone else was eating. Weight loss is another hidden danger. People on strict low-protein diets often lose muscle without realizing it. They think they’re just eating "lighter," but their strength fades. That increases fall risk-the leading cause of injury in Parkinson’s.
How to Do It Right
You don’t have to figure this out alone. The best outcomes happen when you work with a dietitian who understands Parkinson’s. Here’s what works:- Track your meals and symptoms: Use an app like MyFitnessPal to log protein grams and note your "on/off" times. Look for patterns. Does your hand shake more after pasta with tomato sauce? Maybe the sauce had hidden protein from cheese or meat broth.
- Start with PRD: Try keeping breakfast and lunch under 7g of protein. Use eggs (1 egg = 6g), fruit, oats, rice cakes, and vegetables. Save chicken, fish, tofu, or beans for dinner.
- Time your pills: Take levodopa 30-45 minutes before breakfast and lunch. Wait at least 60 minutes after eating protein before taking your next dose.
- Watch your weight: Weigh yourself weekly. If you lose more than 1kg in two weeks, talk to your doctor. You may need to adjust your protein plan.
- Check for deficiencies: Long-term protein restriction can lower vitamin B12 and iron. Get blood tests every 6 months.
Who Should Avoid This?
Not everyone needs to change their diet. If you’re underweight (BMI under 20), have a history of malnutrition, or are already losing muscle, protein restriction could hurt you more than help. Also, if you’ve only been on levodopa for less than 5 years and don’t have motor fluctuations, you likely don’t need to change anything yet. The interaction usually develops over time. The key is personalization. As Dr. Carley Rusch says, "It’s not one size fits all." Some people can handle a small amount of protein with their pill. Others need strict PRD. Only testing and tracking will tell you what works for you.What’s Next?
Researchers are working on better solutions. One new approach, called "protein pacing," is in clinical trials. Instead of cutting protein or moving it to nighttime, it gives small amounts every few hours to keep amino acid levels steady-so they don’t spike and block levodopa. Early results show 68% of participants improved their symptoms and stuck with the plan longer than with PRD. Another idea: new forms of levodopa that bypass the LAT1 transporter entirely. If they work, they could make protein diets irrelevant. But for now, PRD is your best tool. It’s not easy. But for many, it’s the difference between being stuck on the couch and walking to the park.Can I still eat meat if I take levodopa?
Yes-but timing matters. Eat meat in the evening, at least 60 minutes after your last levodopa dose of the day. Avoid meat at breakfast or lunch, when levodopa absorption is most critical. A 100g chicken breast has about 30g of protein-enough to interfere with your medication if eaten too close to a dose.
Does dairy affect levodopa the same way as meat?
Yes. Milk, cheese, yogurt, and other dairy products are high in protein and contain the same amino acids that compete with levodopa. One cup of milk has 8g of protein. A slice of cheddar has 7g. They’re not "safe" just because they’re not meat. Treat dairy like any other protein source and avoid it during daytime meals if you’re using PRD.
What are good low-protein breakfast options?
Try oatmeal with fruit and honey, rice cakes with jam, fruit smoothies made with water or juice (not milk), toast with avocado or jam, or vegetable soups without beans or broth made from meat. Avoid eggs, yogurt, and protein shakes. Even peanut butter has about 8g per 2 tablespoons-so use it sparingly.
How long does it take to see results from a protein redistribution diet?
Most people notice changes in 2-4 weeks. You might feel more consistent mobility in the morning or fewer sudden "off" episodes after lunch. But it takes 3-6 weeks to fully adjust your meals and track patterns. Keep a daily log of what you ate and how you felt. That’s the key to knowing if it’s working for you.
Is it safe to try this on my own?
You can start tracking your meals and symptoms on your own, but working with a dietitian is strongly recommended. A 2022 study found that 78% of people who got professional help improved their symptom control, compared to only 32% who tried alone. Dietitians can help you avoid weight loss, nutrient gaps, and social burnout. They can also help you adapt the plan to your culture, favorite foods, and lifestyle.

steve rumsford
January 7, 2026 AT 12:03so i tried eating only rice and bananas all day and took my meds before breakfast and still froze mid-step walking to the fridge. like bro. this is a nightmare.
Poppy Newman
January 8, 2026 AT 19:07the protein redistribution diet sounds like a dream if you’re single and live alone. but try explaining to your mom why you’re not eating her lasagna on Sunday. 😔
Alex Danner
January 10, 2026 AT 03:26the science here is solid. LAT1 transporters are the bottleneck. it’s not about being ‘diet-obsessed’-it’s about pharmacokinetics. the body doesn’t care if you ‘love steak.’ it cares about leucine concentration in plasma. if your levodopa isn’t working after lunch, protein is almost always the cause. track it for two weeks. use a food scale. you’ll be shocked.
also-dairy is just as bad. cheese, milk, yogurt. all full of those same amino acids. people think ‘it’s just a glass of milk’ but 8g of protein = 30% drop in absorption. that’s not a snack. that’s a medical event.
the 2017 study showing PRD reduces off-time by nearly two hours? replicated across three continents. this isn’t anecdotal. it’s clinical. and yet, so many docs still don’t mention it. why? because nutrition isn’t in med school curricula. so you have to be your own advocate.
start small. skip the eggs at breakfast. swap yogurt for fruit. use rice cakes instead of toast with peanut butter. it’s not starvation. it’s strategy.
and yes, you can still eat meat. just not at 8am. save it for 7pm. your brain will thank you.
Mina Murray
January 10, 2026 AT 12:55oh great. so now we’re supposed to become nutritionists on top of managing a neurodegenerative disease? next they’ll tell us to meditate and do yoga to ‘balance our dopamine.’
this is just another way pharma wants us to blame ourselves. what if the real problem is that levodopa is a 60-year-old drug with terrible bioavailability? why aren’t we pushing for better meds instead of making people eat rice cakes for life?
and who even made up this ‘protein redistribution’ nonsense? some dietitian who’s never held a tremoring hand?
my uncle lost 18 pounds in 4 months doing this. his legs gave out. he fell. broke his hip. now he’s in a nursing home. so thanks for the ‘solution.’
Vince Nairn
January 12, 2026 AT 10:39so let me get this straight-you’re telling me i can’t eat my damn chicken sandwich at lunch but i can have a whole ribeye at 8pm? that’s not a diet. that’s a punishment.
and who’s gonna cook two separate meals? my wife’s already tired of being a nurse. now she’s gotta be a protein accountant too?
also, i’ve been on levodopa for 11 years. i eat steak every day. i’m still walking. maybe this ‘science’ doesn’t apply to everyone.
or maybe the real problem is your doctor doesn’t know what they’re talking about.
LALITA KUDIYA
January 12, 2026 AT 14:24i tried PRD for 3 months. i felt better in the morning. but i missed my family dinners so much. now i just take my meds after dinner and deal with the off-periods. it’s not perfect. but i’m still here. and i’m still eating curry. ❤️
Jonathan Larson
January 14, 2026 AT 09:44The empirical evidence supporting protein redistribution is robust, and its clinical utility is well-documented in peer-reviewed literature spanning multiple cohorts. The competition between large neutral amino acids and levodopa for the LAT1 transporter is not speculative-it is a well-characterized pharmacological interaction. To dismiss it as anecdotal is to misunderstand the foundational principles of neuropharmacology.
Moreover, the social and psychological toll of dietary modification must be acknowledged with equal rigor. The isolation experienced by patients who cannot partake in communal meals is a legitimate comorbidity. A truly holistic approach must integrate nutritional science with psychosocial support, ideally through multidisciplinary care teams that include dietitians, occupational therapists, and mental health professionals.
It is not merely about extending ‘on’ time. It is about preserving dignity, autonomy, and connection to the social fabric of life. This is not a dietary hack. It is a matter of neuroethical care.
Kamlesh Chauhan
January 15, 2026 AT 05:41why are we even talking about this? the real problem is that levodopa is outdated. they’ve had better drugs for 20 years but they don’t want to sell them because they’re too expensive. this protein stuff is just a distraction. big pharma wants you to think you can fix this with rice cakes instead of paying for real medicine.
also my cousin’s neighbor’s dog has parkinson’s and it eats steak every day and runs around like a puppy. so maybe this is all fake.
Kyle King
January 16, 2026 AT 13:07you know what’s really happening? the government and the pharmaceutical companies are in cahoots. they want you to eat low-protein meals so you’ll be weaker, less active, and more dependent on their meds. this ‘protein redistribution’ is just a way to keep you docile. they don’t want you strong. they want you compliant.
and why is everyone suddenly talking about ‘LAT1 transporters’? because they read one article. you think your brain is the only one affected? what about your liver? your kidneys? they’re probably being poisoned by this diet too.
if you really want to fix this, stop taking the pills. go to a naturopath. drink green tea. meditate. the body heals itself.
Andrew N
January 18, 2026 AT 08:37i tried the protein thing. didn’t work for me. maybe i’m just lucky. or maybe the science is wrong. i eat protein with my meds and i’m fine. so maybe it’s not for everyone. just saying.
Rachel Steward
January 18, 2026 AT 22:17you all are missing the point. this isn’t about protein. it’s about control. they’re making you change your life to fit a 1960s drug. they’re not fixing the problem. they’re making you adapt to it. that’s not progress. that’s surrender.
and why do you think the ‘protein redistribution diet’ works for some? because they’re already disciplined. the rest of us? we’re just trying to survive. we don’t have time to track grams of leucine. we’re tired. we’re in pain. we just want to eat a sandwich without feeling like a lab rat.
this isn’t science. it’s guilt dressed up as advice.
steve rumsford
January 19, 2026 AT 10:07just ate a steak at 7pm. took my pill at 8. felt better at 9. i’m not a scientist. but i know what works. this is my life. not a textbook.