Reading a prescription label isn’t just about knowing how much to take or when. For people with food allergies or sensitivities, it’s a life-or-death task. The ingredients list on your pill bottle might include milk, soy, or peanuts - not as active drugs, but as inactive ingredients that can trigger severe reactions. Unlike food, where allergens are clearly labeled by law, medicines have no such rules. That means you can’t assume safety just because the label doesn’t say "contains peanuts." You have to dig deeper.
Why Prescription Labels Don’t Tell You Everything
The Food Allergen Labeling and Consumer Protection Act (FALCPA) forces food companies to spell out the nine major allergens: milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. But that law doesn’t apply to pills, creams, or injections. The FDA doesn’t require drug manufacturers to list allergens in inactive ingredients - even if those ingredients come from allergenic sources. For example, lactose (a milk sugar) is used in over 20% of oral medications. Soy lecithin, often found in capsules, is a common emulsifier. Peanut oil, though rare, still shows up in some injectables. These aren’t listed as "peanut" or "milk." They’re hidden under technical names like "lactose monohydrate" or "soybean oil." And if you don’t know what those terms mean, you’re flying blind.How to Spot Hidden Allergens on Medicine Labels
Start by looking at the inactive ingredients section. It’s usually on the package insert, inside the box, or sometimes printed on the bottle label. If you can’t find it, ask your pharmacist for a copy of the full prescribing information. Don’t rely on the front label - it often only lists the active drug. Here’s what to look for:- Lactose = milk derivative
- Soy lecithin or soybean oil = soy
- Arachis oil = peanut oil
- Casein or whey = milk proteins
- Starch = could be corn, wheat, or potato (wheat starch is a known allergen)
- Food colorings like FD&C Yellow No. 5 or red dye #40 may be processed with allergenic carriers
What to Do When the Label Is Unclear
Pharmacists are your best ally. They have access to databases that list every ingredient in every generic and brand-name drug. Ask them: "Does this medication contain milk, soy, peanuts, or wheat?" Don’t say "Does it have allergens?" - be specific. Generic versions of the same drug can have completely different inactive ingredients depending on the manufacturer. A pill you’ve taken safely for years might suddenly change suppliers - and with it, its allergen profile. If you’re unsure, request a medication guide from your pharmacist. These are printed sheets that list all ingredients in plain language. Some pharmacies now offer digital versions you can access through their app. If your pharmacy doesn’t provide this, ask for a printout. It’s your right.Food vs. Medicine: The Labeling Gap
Food labels have to follow strict rules. If a product contains almonds, it must say "almonds" in parentheses or in a "Contains" statement. Medicines don’t. This gap is dangerous. Over 4% of U.S. adults have a known allergy to at least one medication ingredient, and many don’t realize it’s tied to food allergies. People allergic to soy might react to soy lecithin in a pill. Those allergic to milk might not know lactose is in their blood pressure med. A 2022 FDA report showed that 87% of patients with food allergies never asked their doctor or pharmacist about inactive ingredients in prescriptions. That’s not laziness - it’s lack of awareness. Most people assume if it’s a pill, it’s safe. It’s not.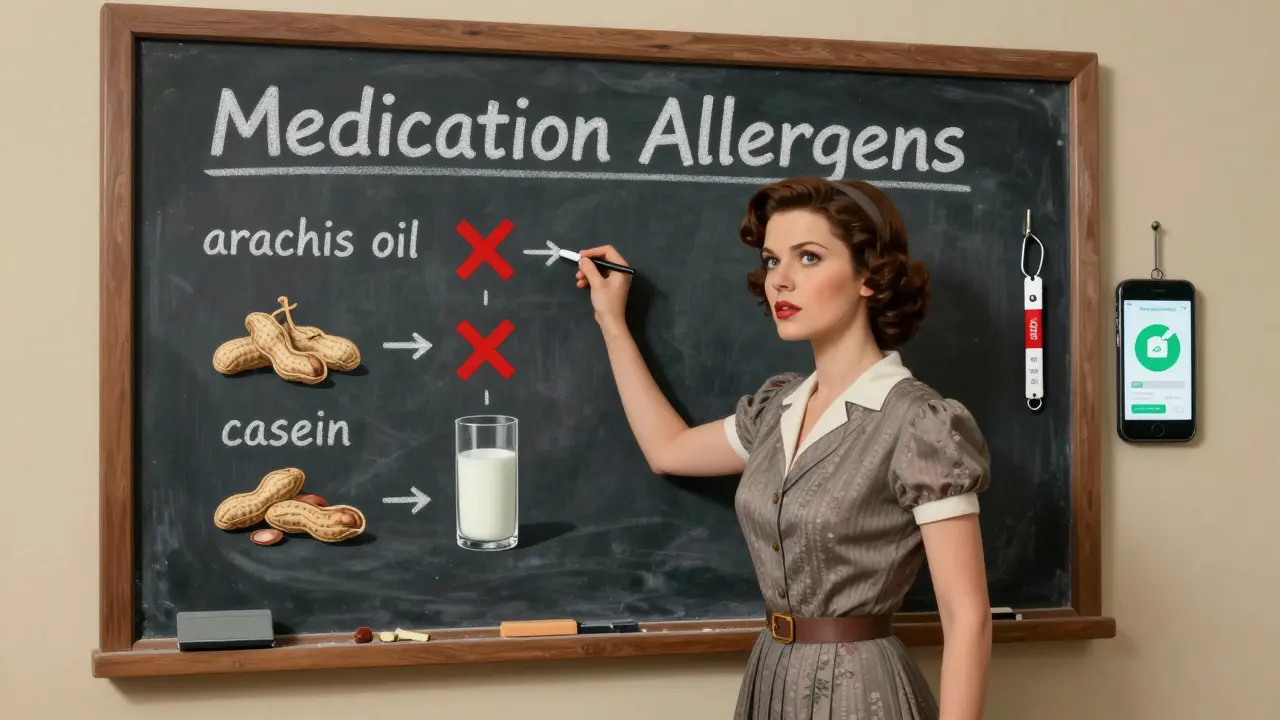
How to Stay Safe Long-Term
Build a personal list of allergens you avoid - and their hidden names. Keep it on your phone or printed out. Update it every time you get a new prescription. Use apps like AllergyEats’ Scan feature (launched in early 2024) to take a photo of your pill bottle’s ingredient list. The app can flag potential allergens with 92% accuracy. Always check the label before taking any new medication - even if it’s the same drug you’ve taken before. Manufacturers change fillers all the time. FARE’s 2022 report found that 28% of accidental reactions came from formulations that changed without warning. If you’ve had a reaction before, wear a medical alert bracelet that lists your medication allergens. Tell every new doctor and pharmacist about them - even if you think it’s unrelated. Your primary care provider might not know that your asthma inhaler contains lactose.What’s Changing in 2025 and Beyond
The FDA is considering new rules to standardize allergen labeling on drugs. A proposed rule published in May 2024 could require manufacturers to list allergens in a consistent format, similar to food. It’s still in review, but if passed, it would be the biggest change in medication labeling since the 1990s. In the meantime, the burden is on you. Don’t wait for the system to fix itself. Learn the names. Ask questions. Keep records. Your life depends on it.Are inactive ingredients always listed on prescription labels?
No. Inactive ingredients are often listed only in the package insert or prescribing information, not on the front of the bottle. Always ask your pharmacist for the full ingredient list if you have allergies.
Can generic drugs have different allergens than brand-name versions?
Yes. Generic drugs must contain the same active ingredient, but they can use different fillers, binders, or coatings. One generic version might use lactose; another might use corn starch. Always check the ingredients when switching generics.
What should I do if I have a reaction to a medication?
Stop taking the medication immediately and contact your doctor. Report the reaction to the FDA’s MedWatch program. Then, ask your pharmacist to identify the ingredient that caused the reaction so you can avoid it in the future.
Is sesame a concern in medications?
Yes. While sesame is now a required allergen on food labels since 2023, it’s still not required on medicine labels. Sesame oil or sesame-derived emulsifiers can appear in capsules or injectables. Always ask if you’re allergic to sesame.
How can I find out what’s in my medication if the label doesn’t say?
Call your pharmacy and ask for the full prescribing information or package insert. You can also search the drug name plus "inactive ingredients" on the FDA’s DailyMed website. Never guess - if you’re unsure, assume it contains an allergen until proven otherwise.

Solomon Ahonsi
February 2, 2026 AT 15:07This is such a fucking joke. You expect people to memorize chemical names like it's a college exam? I just want to take my damn pill without doing a PhD in pharmacology. The system is broken and nobody gives a shit.
George Firican
February 2, 2026 AT 22:48There’s a profound irony in how we regulate the peanut butter on our toast with military precision, yet allow the same allergens to lurk in the very substances meant to heal us. The disconnect isn’t accidental-it’s a reflection of how medicine prioritizes cost and convenience over bodily autonomy. We treat drugs like commodities, not lifelines. The silence around inactive ingredients isn’t oversight; it’s systemic neglect dressed in regulatory jargon.
Matt W
February 2, 2026 AT 23:33Just had to call my pharmacist yesterday because my new generic BP med made my throat itch. Turned out it had lactose. I didn’t even know that was a thing. Thanks for this post-it saved me from another trip to the ER. Seriously, everyone with allergies: ask for the insert. Don’t trust the bottle.
Akhona Myeki
February 4, 2026 AT 18:06It is utterly unacceptable that Canada and the United States permit such reckless disregard for public health. In South Africa, we do not allow such negligence in pharmaceutical manufacturing. The FDA must be held accountable. This is not merely an oversight-it is a violation of the most basic human right: the right to safe medication.
Sandeep Kumar
February 5, 2026 AT 20:20Vatsal Srivastava
February 7, 2026 AT 08:19Brittany Marioni
February 9, 2026 AT 03:27Thank you so much for sharing this!! I’m so glad someone is finally talking about this!! So many people don’t realize that even "natural flavors" can be hiding allergens!! I’ve had reactions to meds because I assumed "filler" meant harmless!! Please, everyone-keep a list!! Update it!! And don’t be shy to ask your pharmacist-they’re trained for this!!
Nick Flake
February 9, 2026 AT 13:15This post hit me right in the soul 🥺 I’ve had anaphylaxis from a pill I’d taken for 5 years-because the manufacturer switched from corn starch to wheat starch. No warning. No label change. Just… chaos. I now have a laminated card in my wallet with every allergen and its sneaky aliases. I’m not just surviving-I’m educating. This isn’t paranoia. It’s precision.
Bob Hynes
February 10, 2026 AT 00:32Man I just read this while waiting for my prescription and damn… I never thought about arachis oil being peanut. I thought that was just some fancy french word for oil. Like, I’m Canadian but I feel like I’ve been living in a bubble. Gonna print this out and stick it on my fridge. Also, the app thing? That’s actually kinda cool. I’m gonna try it.
Eli Kiseop
February 11, 2026 AT 03:20Ellie Norris
February 11, 2026 AT 18:52Oh my gosh, I just realised my eczema cream has lanolin-sheep’s wool derivative! I’m allergic to wool and never connected the dots! Thank you for this-I’m going to call my pharmacist right now and ask for a new one. I think I’ve been misdiagnosing my flare-ups as stress for years… 🙈