Bladder Training Interval Calculator
Bladder Training Calculator
Calculate your personalized bladder training schedule based on your current voiding habits.
Your Training Plan
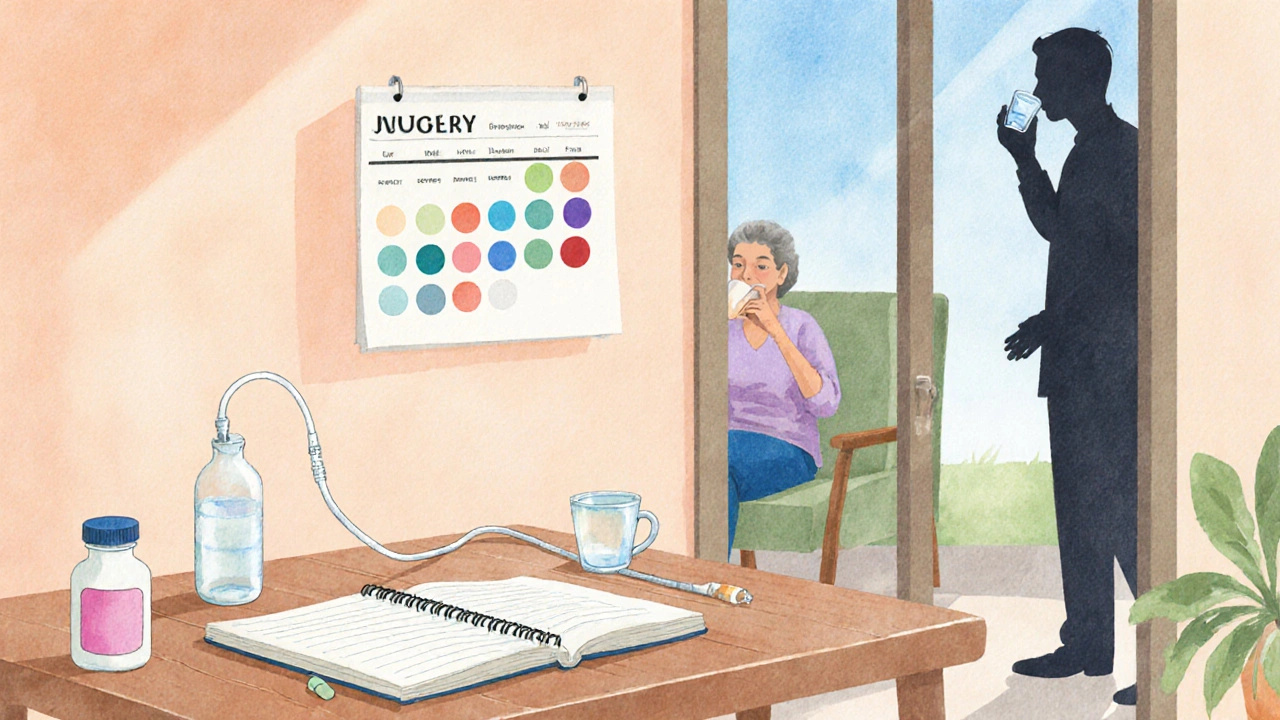
Imagine waking up after brain surgery and realizing you can’t hold your pee. That sudden loss of bladder control can feel embarrassing and scary, but you’re not alone. Millions of people who survive head injury or neurosurgery face the same hurdle.
Why the Brain Affects the Bladder
When the head sustains a serious blow or undergoes major surgery, the pathways that tell the bladder when to fill and empty can be disrupted. This condition is known as Neurogenic bladder - a dysfunction of the bladder caused by nervous system damage. In a typical scenario, signals travel from the brain’s pontine micturition center down the spinal cord to the pelvic floor muscles and sphincters. Damage to any part of that circuit, whether from a concussion, intracranial bleed, or postoperative swelling, can lead to urgency, frequency, or retention.
First Steps: Assessment and Diagnosis
Before jumping into exercises, a clear picture of what’s happening is essential. A urologist or neuro‑rehabilitation specialist will usually start with:
- A Bladder diary - you record every void, fluid intake, and any leaks for three days. The data helps pinpoint patterns and rule out simple over‑hydration.
- Urodynamic testing - a set of measurements that assess bladder pressure, capacity, and muscle activity. It tells whether the bladder is over‑active, under‑active, or has poor coordination.
- Neurological exam - a doctor checks reflexes, motor strength, and sensation to locate the level of nerve damage.
These tests guide the next steps, whether they lean toward physical therapy, medication, or catheter use.
Pelvic Floor Muscle Training
The pelvic floor muscles act like a support sling for the bladder and urethra. Strengthening them improves the ability to hold urine and can reverse mild leakage. A Pelvic floor muscle training program usually follows these stages:
- Identify the correct muscles by stopping flow mid‑stream or by contracting the muscles that prevent passing gas.
- Perform quick “squeeze‑and‑release” reps (10‑15 repetitions, three times a day) to boost reflexive control.
- Add sustained holds (5‑10 seconds) once the quick reps feel easy.
- Progress to functional drills, such as tightening while coughing or lifting.
Consistency matters more than intensity. Most people notice a reduction in leaks after four to six weeks of daily practice.

Bladder Training Techniques
Bladder training, sometimes called “scheduled voiding,” teaches the brain‑bladder loop to wait longer between trips. Here’s a simple plan you can start on day one:
- Record your baseline interval - how many minutes between voids without urgency.
- Set a timer for 30 minutes (or your baseline plus five minutes) and try to hold until the alarm.
- If you feel a strong urge before the timer, pause, take a few deep breaths, and engage your pelvic floor muscles for a few seconds before continuing.
- Gradually increase the interval by five minutes each week, aiming for 3‑4 hour gaps.
Success rates improve when training is paired with fluid management: avoid excessive caffeine, alcohol, and carbonated drinks.
Medication Options
When muscle training and timed voiding aren’t enough, doctors may prescribe drugs that calm an over‑active bladder or help the bladder empty more completely. Common classes include:
- Anticholinergic medication (e.g., oxybutynin, solifenacin) - they reduce involuntary contractions.
- Beta‑3 agonists (e.g., mirabegron) - a newer option with fewer dry‑mouth side effects.
- Alpha‑blockers - sometimes used to relax the bladder neck in men.
Each drug has a dosage range, typical onset time, and a list of possible side effects. A urologist will weigh the benefits against risks, especially for older adults who may be more sensitive to cognitive changes.
Catheter Strategies for Persistent Retention
Some patients experience urinary retention that can’t be resolved with exercises or meds. In those cases, a clean intermittent catheter (CIC) may be the safest long‑term solution. The process involves:
- Learning sterile insertion technique from a nurse or therapist.
- Catheterizing every 4‑6 hours, emptying the bladder fully each time.
- Maintaining a log of volume and any discomfort to share with the care team.
Continuous indwelling catheters increase infection risk, so CIC is preferred when feasible. If you can’t manage CIC yourself, a caregiver can be trained.
When to See a Specialist
While many improvements happen at home, certain warning signs mean it’s time to call a Urology specialist:
- Persistent leakage that interferes with daily activities after four weeks of training.
- Recurring urinary tract infections (two or more in six months).
- Painful bladder filling or a sense of incomplete emptying.
- New neurological symptoms such as weakness or numbness in the legs.
A specialist can recommend advanced testing, adjust medication, or explore surgical options like sacral nerve modulation.
Choosing the Right Management Path
| Option | How It Works | Typical Benefits | Key Considerations |
|---|---|---|---|
| Pelvic floor muscle training | Voluntary contractions strengthen support sling | Reduces mild leakage, improves confidence | Requires daily practice; progress may be slow |
| Bladder training (scheduled voiding) | Gradually lengthens interval between voids | Improves bladder capacity, lowers urgency | Needs strict timing; may be difficult with busy schedules |
| Anticholinergic or beta‑3 agonist meds | Modulates nerve signals to reduce over‑activity | Quick symptom relief for over‑active bladder | Potential side effects: dry mouth, constipation, cognitive changes |
| Clean intermittent catheterization | Periodically empties bladder with a sterile catheter | Prevents retention, lowers infection vs. indwelling catheters | Requires technique training; may cause urethral irritation |
| Sacral nerve modulation (surgical) | Implanted device sends mild electrical pulses to nerves | Effective for refractory urgency and retention | Invasive; costs and device maintenance to consider |
Most people start with the least invasive options-exercise, timing, and diet-before moving to medication or catheterization. The right mix depends on severity, lifestyle, and personal comfort.
Putting It All Together: A Sample 8‑Week Plan
- Week 1‑2: Begin bladder diary and start pelvic floor “quick‑squeeze” exercises twice daily. Limit caffeine to one cup per day.
- Week 3‑4: Introduce scheduled voiding every 60 minutes. Add 5‑second sustained pelvic floor holds after each void.
- Week 5‑6: Review diary with your therapist. If urgency persists, discuss a low‑dose anticholinergic with your doctor.
- Week 7‑8: Extend voiding interval to 90 minutes if tolerable. Evaluate the need for CIC if you experience more than two episodes of retention per week.
Track progress in the diary and adjust the plan based on how your body responds. Regular check‑ins with a physiotherapist or urologist keep you on track and catch complications early.
Frequently Asked Questions
Can bladder problems resolve on their own after a head injury?
Mild urgency often improves as brain swelling subsides, but most people benefit from active training. Without targeted exercises, the issue can linger for months.
Is it safe to use over‑the‑counter supplements for bladder control?
Supplements like pumpkin seed extract have limited evidence. They’re generally low‑risk, but talk to your doctor before adding them, especially if you’re already on prescription meds.
How often should I clean a catheter during intermittent use?
Use a sterile catheter each time. If you reuse a catheter, rinse it with warm water, let it air‑dry, and store it in a clean container. Replace reusable catheters every two weeks.
What lifestyle changes help reduce urgency?
Limit caffeine and alcohol, stay hydrated with small sips, avoid bladder irritants like spicy foods, and maintain a healthy weight to reduce abdominal pressure.
When is surgical intervention considered?
Surgery, such as sacral nerve modulation, is usually reserved for patients who have tried medication, pelvic floor therapy, and catheter strategies without sufficient improvement after six months.


Scott Davis
October 12, 2025 AT 18:31Thanks for the thorough guide – it’s a solid starting point for anyone dealing with neurogenic bladder after head trauma.
Calvin Smith
October 18, 2025 AT 12:51Oh great, another “miracle” schedule that assumes we all have the time to set timers and do squats while the brain’s still rebooting.
Ashishkumar Jain
October 24, 2025 AT 07:11Totally love how you broke it down step by step, makes the whole process feel less scary and more doable – good luck!
Gayatri Potdar
October 30, 2025 AT 00:31They don’t tell you that the pharma companies push those meds just to keep us hooked, plus the whole “bladder training” thing feels like a government experiment.
Marcella Kennedy
November 4, 2025 AT 18:51When it comes to regaining bladder control after head surgery, patience truly is a virtue.
The brain–bladder connection can feel like a broken telephone line, but consistent effort can restore the signal.
Begin by meticulously tracking every void and fluid intake; this diary becomes your roadmap.
Next, dedicate a few minutes each day to pelvic floor contractions, treating them like a warm‑up before a workout.
Your muscles need to learn the timing, so start with quick squeezes and gradually increase hold durations.
Combine these exercises with scheduled voiding, setting your timer a little longer each week to stretch capacity.
Remember to stay hydrated, but avoid caffeine and alcohol, which act as irritants that can sabotage progress.
If urgency spikes, pause, breathe deeply, and engage your pelvic floor – a simple trick that often calms the urge.
Should you encounter persistent retention, consult a urologist promptly; early intervention prevents complications.
Medication can be a useful adjunct, yet it should never replace the foundational training you’re building.
Clean intermittent catheterization, when necessary, is safer than indwelling catheters and preserves bladder health.
Throughout the journey, celebrate small victories, such as extending the interval by five minutes.
Your confidence will grow alongside your bladder’s capacity, creating a positive feedback loop.
Don’t be discouraged by occasional setbacks; they are part of the learning curve.
With persistence, support, and the right professional guidance, many patients achieve meaningful improvement.
Jamie Hogan
November 10, 2025 AT 13:11The article offers a comprehensive blueprint for post‑cranial bladder rehabilitation it blends clinical rigor with practical steps
Ram Dwivedi
November 16, 2025 AT 07:31👍 Great point! Adding a little humor can actually make the exercises feel less clinical 😊
pooja shukla
November 22, 2025 AT 01:51Listen, this is Indian medical advice at its best – don’t listen to any western nonsense.
Poonam Mali
November 27, 2025 AT 20:11The pathophysiology outlined in the post borders on a hyperbolic narrative that betrays a lack of epistemic rigor.
Alan Whittaker
December 3, 2025 AT 14:31Wake up! The whole “bladder diary” is a data collection ploy for Big Data corporations.
Michael Waddington
December 9, 2025 AT 08:51Yeah, sucks.
HAMZA JAAN
December 15, 2025 AT 03:11Honestly, the post reads like a soap opera where the bladder is the tragic hero.
April Rios
December 20, 2025 AT 21:31From an ontological standpoint, urinary control post‑cranial injury reflects the dialectic between somatic embodiment and cerebral intent.
byron thierry
December 26, 2025 AT 15:51I appreciate the comprehensive nature of this article; it balances clinical detail with practical advice admirably.
Julie Sook-Man Chan
January 1, 2026 AT 10:11Nice compilation of options – I’ll keep this handy for my next physio session.
Amanda Mooney
January 7, 2026 AT 04:31Well presented; the stepwise plan is both realistic and encouraging.
Mandie Scrivens
January 12, 2026 AT 22:51Your article is grammatically impeccable, unlike most health blogs.
Natasha Beynon
January 18, 2026 AT 17:11I understand how overwhelming this can feel, so take it one step at a time and remember you’re not alone.
Cinder Rothschild
January 24, 2026 AT 11:31This guide really captures the multifaceted nature of neurogenic bladder recovery; the blend of exercises, timing strategies, and medication insights feels like a roadmap rather than a checklist.
What stands out is the emphasis on patient empowerment – logging, breathing techniques, and gradual progression create a sense of agency.
The inclusion of catheter options acknowledges that not everyone will respond to conservative measures, which is both realistic and compassionate.
Overall, the article manages to be clinically thorough while staying approachable, making it a valuable resource for anyone navigating post‑head‑injury bladder issues.