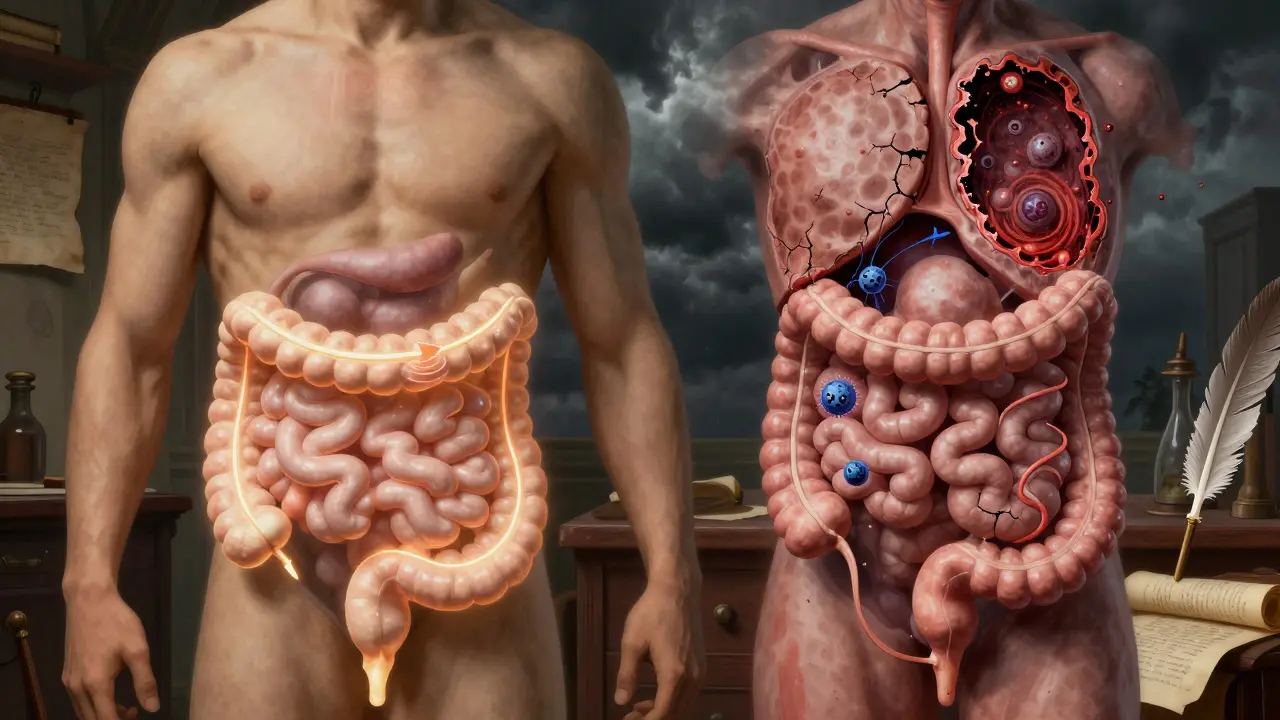
It’s easy to confuse IBS and IBD. Both cause stomach pain, bloating, diarrhea, and cramps. But they’re not the same thing-and knowing the difference matters a lot. One is a functional disorder, meaning your gut looks normal but doesn’t work right. The other is an inflammatory disease, where your intestines are actually damaged. Mixing them up can lead to wrong treatments, unnecessary tests, or even missed warning signs.
What Is IBS? A Gut That Misfires
IBS, or Irritable Bowel Syndrome, is like a glitch in your gut’s software. There’s no infection, no ulcer, no swelling. Your colon looks perfectly fine on a colonoscopy. But it doesn’t handle food, gas, or stress the way it should. Think of it like a misbehaving thermostat: everything’s connected, but the signals are off.
The Rome IV criteria, updated in 2016, define IBS by three main things: abdominal pain at least once a week for three months, plus changes in bowel habits. That means either too many trips to the bathroom, too few, or a mix of both. Bloating hits 76% of people with IBS. Mucus in stool? That’s common too-seen in nearly half of cases. And it usually gets worse after eating.
Here’s the key: IBS doesn’t cause physical damage. No scarring. No bleeding. No cancer risk. Blood tests, stool tests, and colonoscopies all come back normal. That’s why doctors call it a functional disorder. It’s real pain, real discomfort, but not from tissue damage.
What Is IBD? When Your Gut Is Under Attack
IBD-Inflammatory Bowel Disease-isn’t just a glitch. It’s war. Your immune system attacks your own digestive tract. There are two main types: Crohn’s disease and ulcerative colitis. Both cause chronic inflammation. And that inflammation doesn’t just hurt-it destroys.
Crohn’s can strike anywhere from mouth to anus. It digs deep, creating ulcers, strictures (narrowed areas), and fistulas (abnormal tunnels between organs). Ulcerative colitis sticks to the colon and rectum, but it tears through the inner lining, causing open sores. That’s why bloody stool is so common-92% of ulcerative colitis patients have it at diagnosis. You might also see black, tarry stools, which mean bleeding higher up in the gut.
Other red flags? Unexplained weight loss, fever, fatigue. And outside the gut? IBD can cause joint pain, eye inflammation (uveitis), skin rashes like erythema nodosum, and liver issues. These aren’t random. They’re signs your immune system is in overdrive.
The Big Difference: Inflammation vs. No Inflammation
This is where everything splits. IBD shows up on tests. IBS doesn’t.
Doctors use two simple blood and stool markers to tell them apart: CRP and fecal calprotectin. CRP is a general inflammation flag. In active IBD, it’s almost always over 5 mg/L. Normal is under 3. Fecal calprotectin? That’s a protein released by white blood cells in the gut. In IBD, levels jump above 250 µg/g. In IBS? They stay below 50 µg/g-normal.
Colonoscopy is the gold standard. In IBD, you’ll see red, swollen tissue, ulcers, bleeding, or scarring. In IBS? The lining looks healthy. No changes. No damage. That’s why doctors don’t just rely on symptoms. They rule out inflammation first.
The CDC and Mayo Clinic both say it clearly: IBD causes structural damage. IBS does not. If you’re losing weight, having blood in your stool, or running a fever, you’re not dealing with IBS alone. You need urgent evaluation.

Diagnosis: How Doctors Tell Them Apart
Diagnosing IBS is like solving a mystery with no crime scene. You eliminate everything else. That’s called a diagnosis of exclusion. If your blood tests are clean, your stool tests show no infection or inflammation, your colonoscopy looks normal, and you don’t have alarm signs like rectal bleeding or family history of colon cancer-you’re likely diagnosed with IBS.
IBD diagnosis is the opposite. It’s about finding proof of damage. Doctors start with blood and stool tests. If CRP or calprotectin is high, they move to imaging. MRI enterography can show thickened bowel walls and fistulas in Crohn’s. A colonoscopy with biopsy is the final step. In IBD, the tissue under the microscope shows immune cells, ulcers, and inflammation. No guesswork.
And here’s something people don’t realize: you can have both. About 22% to 35% of IBD patients in remission still meet IBS criteria. Their gut is healed enough to stop bleeding and inflammation, but still overly sensitive. That’s why treating IBD doesn’t always fix all symptoms.
Treatment: Different Goals, Different Tools
IBD treatment is about stopping the fire. You need drugs that calm the immune system. Anti-TNF drugs like infliximab work for half of Crohn’s patients within weeks. Corticosteroids help in flares, but you can’t stay on them forever-they wreck your bones and hormones. Newer biologics like vedolizumab target only the gut, reducing side effects. In severe cases, surgery removes damaged parts of the intestine.
IBS treatment? It’s about calming the nerves and adjusting the gut. No immune drugs. No surgery. Instead, diet plays a huge role. The low-FODMAP diet reduces gas, bloating, and pain in 76% of people. It cuts out certain carbs that ferment in the gut-onions, garlic, beans, apples, milk. It’s not a cure, but it’s a game-changer.
Low-dose antidepressants? Yes. Not because you’re depressed. Because they help block pain signals from the gut to the brain. Tricyclics like amitriptyline reduce pain in 60% of IBS patients. Medications like eluxadoline help with diarrhea-predominant IBS. Probiotics, stress management, and gut-directed hypnotherapy also show strong results.

Long-Term Risks: What You’re Really Up Against
IBS doesn’t turn into cancer. It doesn’t cause bowel obstructions. It doesn’t lead to hospitalization from complications. But it can wreck your life. People with IBS report giving up coffee, travel, sex, even phone use just to avoid flare-ups. It’s not just physical-it’s emotional, social, exhausting.
IBD? The stakes are higher. After 10 years of pancolitis (inflammation across the whole colon), the risk of colorectal cancer jumps 2% per year. Toxic megacolon-a life-threatening dilation of the colon-happens in 2-4% of severe ulcerative colitis cases. Strictures can block your intestine. Fistulas can drain into other organs. Some people need permanent colostomies.
That’s why early, accurate diagnosis is critical. Treating IBS like IBD means putting someone on powerful immunosuppressants they don’t need. Treating IBD like IBS? That’s dangerous. Delayed treatment can mean irreversible damage.
When to See a Doctor
Not every stomach ache is IBS. If you have any of these, see a doctor now:
- Blood in your stool or black, tarry stools
- Unexplained weight loss
- Fevers that come and go
- Family history of colon cancer or IBD
- Symptoms starting after age 50
- Anemia (fatigue, pale skin, dizziness)
These are IBD red flags. They’re not IBS symptoms. And they’re not something to wait out.
For IBS, see a doctor if symptoms are disrupting your life, if over-the-counter fixes don’t help, or if you’re unsure. A proper diagnosis means you can stop guessing and start managing.
Can IBS turn into IBD?
No. IBS cannot turn into IBD. They are completely different conditions with different causes. IBS is a functional disorder with no inflammation or tissue damage. IBD is an inflammatory disease with visible structural damage. While you can have both at the same time, one does not cause or evolve into the other. The Crohn’s & Colitis Foundation and CDC both confirm this.
Is IBD an autoimmune disease?
Yes, IBD is considered an autoimmune condition. In Crohn’s disease and ulcerative colitis, the immune system mistakenly attacks the lining of the digestive tract, causing chronic inflammation. This is different from IBS, which has no autoimmune component. That’s why IBD treatments target immune suppression, while IBS treatments focus on symptom relief.
Can stress cause IBS or IBD?
Stress doesn’t cause either condition, but it can make both worse. In IBS, stress heightens gut sensitivity and changes bowel motility, triggering pain and diarrhea. In IBD, stress can trigger flares by affecting immune activity. Managing stress through therapy, exercise, or mindfulness helps both conditions-but it won’t cure them.
Do I need a colonoscopy if I have IBS symptoms?
If you’re under 50 and have typical IBS symptoms-no blood, no weight loss, no fever-you likely don’t need one right away. But if you have alarm signs, or if you’re over 50, a colonoscopy is strongly recommended to rule out IBD or colon cancer. It’s not about the pain-it’s about eliminating dangerous causes.
Can diet cure IBD?
No diet can cure IBD. While the low-FODMAP diet helps manage symptoms in some IBD patients, especially during remission, it doesn’t stop inflammation. IBD requires medical treatment-immunosuppressants, biologics, or sometimes surgery. Diet is a support tool, not a replacement.

Suzette Smith
February 12, 2026 AT 20:24Okay but what if IBS is just IBD that hasn’t gotten around to showing up on scans yet? I’ve seen people go from ‘oh it’s just IBS’ to full-blown Crohn’s in 18 months. Doctors are too quick to label things as ‘functional’ because they don’t want to order more tests. I’m not saying it’s conspiracy, but… have you ever heard of a patient who got better after going gluten-free and then came back with a fistula? Yeah. Me too.
steve sunio
February 14, 2026 AT 01:11ibd is just a fancy way of saying ur body is broken. ibs is just ur gut being dramatic. stop overmedicating urself. i had diarrhea for 3 weeks once and i just drank gatorade and slept. now i live. u guys need to chill.
Neha Motiwala
February 15, 2026 AT 19:49Did you know the pharmaceutical industry funds 87% of IBS research? And they don’t want you to know that IBD is actually caused by 5G towers and glyphosate in your tap water. My cousin’s neighbor’s yoga instructor’s dog had a colonoscopy and the vet said the lining looked ‘off’-and guess what? She started having symptoms after her smart fridge updated. You think your ‘normal’ colonoscopy is real? Think again.
Also, why are all the doctors white? Why are all the studies based on Americans? I’ve been having cramps since I ate mangoes in Delhi in 2017. No one listens. No one cares. This is systemic.
athmaja biju
February 17, 2026 AT 03:50IBS is not a disease. It is a weakness. In India, we have people who walk 15km daily, eat spicy food at 3am, drink tap water, and never complain. You sit on a chair all day, eat avocado toast, and cry because you have bloating? That’s not a medical condition. That’s a lifestyle failure. You need discipline. Not a low-FODMAP diet.
Also, why is everyone so obsessed with colonoscopies? In my village, we use turmeric and prayer. Works better than biologics.
Robert Petersen
February 17, 2026 AT 08:38This is actually one of the clearest breakdowns I’ve read on this topic. Seriously. You took something that feels overwhelming and made it feel manageable. I’ve been living with IBS for 12 years and I never knew the difference between ‘no damage’ and ‘immune attack’ until now. Thank you for writing this. I’m sharing it with my sister-she’s been terrified she has IBD and this gives her real clarity.
You’re not just explaining medicine. You’re giving people peace.
Craig Staszak
February 17, 2026 AT 11:06Love this breakdown. The calprotectin vs CRP point is gold. I’ve seen so many people get misdiagnosed because they assume ‘if it hurts it’s inflammation’. But your gut can scream without being on fire. That thermostat analogy? Perfect. IBS is like a car alarm going off because someone walked by. IBD is the car actually burning. Both need attention. One needs a mechanic. The other needs firefighters.
Also-yes to gut hypnotherapy. I did 12 sessions. My pain dropped 70%. No drugs. Just voice and breathing. Mind-body stuff isn’t woo. It’s science with soul.
alex clo
February 19, 2026 AT 02:51The distinction between functional and inflammatory disorders is clinically vital. However, the reliance on fecal calprotectin as a standalone diagnostic tool may be premature. Recent studies suggest a false-negative rate of up to 18% in early Crohn’s disease, particularly in ileal involvement. Furthermore, the low-FODMAP diet’s efficacy may be confounded by placebo effects and regression to the mean. A more rigorous, multi-modal diagnostic protocol is warranted.
Alyssa Williams
February 20, 2026 AT 02:45I’ve had IBS since I was 19. 12 years. I tried everything. Low FODMAP. Probiotics. Hypnotherapy. Even that weird tea with mint and ginger. Nothing worked. Then I stopped obsessing. I started walking. I stopped checking my butt every 20 minutes. I stopped Googling. And guess what? My stomach stopped screaming. Not because I cured it. But because I stopped fighting it. You can’t outsmart your gut. You gotta outlive it.
Ernie Simsek
February 21, 2026 AT 00:28IBS is just your gut’s way of saying ‘I’m bored’ 😅 IBD is your gut screaming ‘I’M BEING EATEN ALIVE’ 🔥🔥🔥 I’ve had both. IBD flares = hospital. IBS = me crying in Target because I had to find a bathroom in 3 minutes. Both suck. But one needs a war room. The other needs a nap and a snack.
Also-why do people think diet fixes IBD? Bro. I was on 5 meds. Ate kale. Did yoga. Still had a fistula. Biologics saved me. Not quinoa.
Joanne Tan
February 22, 2026 AT 05:29OMG I just realized I’ve been treating my IBS like IBD for 5 years. I was so scared of ‘something worse’ I kept asking for colonoscopies. My doctor finally said ‘your calprotectin is 12. You’re fine.’ I cried. Not from sadness. From relief. I didn’t need all that drama. I just needed to stop panicking. And yes, the low-FODMAP diet changed my life. No more beans. No more gas. No more ‘I can’t leave the house’ days.
Reggie McIntyre
February 22, 2026 AT 14:43Think of IBS as a miswired Wi-Fi router-everything’s plugged in, signals are scrambled, but the hardware’s pristine. IBD? That’s the router on fire, smoke pouring out, the whole damn house at risk. You don’t fix a router on fire with a factory reset. You grab the extinguisher. And sometimes… you have to replace the whole damn system. The beauty of this distinction is that it saves lives. Not just from pain, but from unnecessary fear. And unnecessary chemo. And unnecessary surgeries. This isn’t just medical trivia. It’s existential clarity.
Carla McKinney
February 23, 2026 AT 09:45This article is dangerously oversimplified. You claim IBS has no cancer risk? What about the 2023 Lancet study showing elevated colorectal adenoma rates in long-term IBS patients? And you dismiss diet as ‘support’ for IBD? Have you heard of the Specific Carbohydrate Diet? It’s been clinically validated in multiple trials. You’re feeding people false reassurance. This isn’t helpful. It’s negligent.
Ojus Save
February 23, 2026 AT 13:12cool post. i had ibs for a while. i just stopped stressing. also i drink more water now. its not that hard.