Inhaler Prevention Checklist
Prevention Risk Assessment
This tool helps you understand your risk of oral thrush and hoarseness from your inhaler. Answer the questions below to get personalized recommendations.
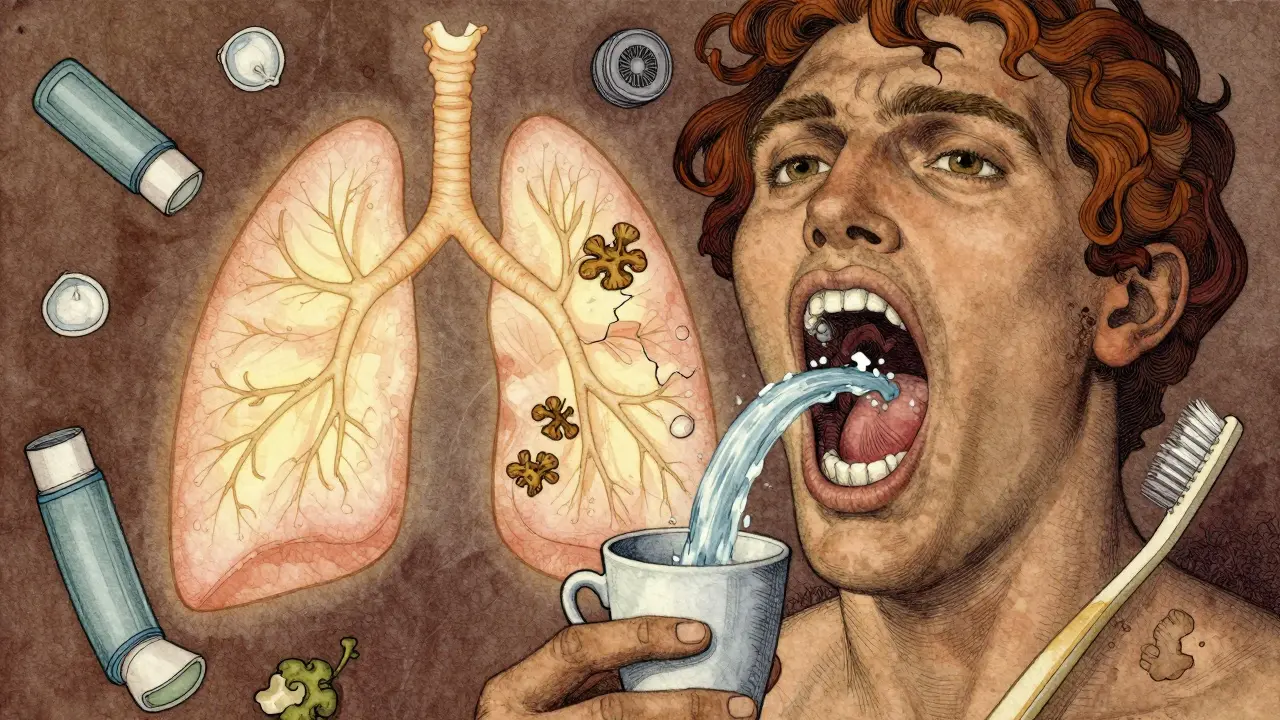
When you use an inhaled corticosteroid for asthma or COPD, you’re doing exactly what your doctor asked: reducing lung inflammation, preventing attacks, and breathing easier. But if you don’t take a few simple steps after each puff, you could end up with a white, patchy mouth or a voice that sounds like gravel. These aren’t rare side effects-they’re common, preventable, and often misunderstood.
Why Your Inhaler Causes Oral Thrush
Inhaled corticosteroids like fluticasone, budesonide, and beclomethasone work by calming down inflammation in your airways. But they don’t just stay in your lungs. A lot of the medicine lands on your tongue, throat, and inner cheeks. That’s not a mistake-it’s how the device works. The problem? Corticosteroids suppress local immune activity. Your mouth has harmless yeast called Candida albicans living in it naturally. Normally, your immune system keeps it in check. But when steroids sit there, they weaken that defense. The yeast overgrows, forming those telltale creamy-white patches. You might not notice at first, but then you feel it: a burning sensation, loss of taste, or pain when eating. Scrape the patch, and you’ll see red, raw tissue underneath. This isn’t just uncomfortable-it can make you avoid your inhaler, which is far more dangerous.
Why Your Voice Gets Hoarse
Hoarseness happens because the same particles that land in your mouth also touch your vocal cords. Corticosteroids cause mild swelling and irritation in the larynx. You might notice your voice cracks, sounds raspy, or disappears entirely after using your inhaler. It usually lasts a few hours, but if you’re using it twice daily, that’s four hours a day of hoarseness. For teachers, singers, or anyone who relies on their voice, this isn’t just annoying-it’s disruptive. And unlike oral thrush, hoarseness doesn’t always come with visible signs. You just know something’s off when you speak.
The Two Most Effective Prevention Strategies
Here’s the truth: you don’t need fancy products or expensive treatments. Two simple habits cut your risk by 60-80%.
- Rinse, gargle, swish, and spit-right after every puff. Don’t swallow. Don’t wait. Do it immediately. Use water. No need for special mouthwashes. Just swish it around your mouth for 20-30 seconds, then spit. Studies show this single step reduces thrush risk by two-thirds. One patient on Asthma.net said, “I got thrush twice before I started rinsing properly. Now I haven’t had it in five years.”
- Use a spacer. If you’re using a metered-dose inhaler (MDI), attach a spacer. It’s a plastic tube that holds the puff of medicine so it doesn’t blast straight into your throat. You breathe in slowly from the spacer, and most of the particles land in your lungs instead of your mouth. Dry powder inhalers (DPIs) are better than MDIs without spacers, but spacers still help even with DPIs. Research from the Healthcare (Basel) review in July 2025 confirms: combining a spacer with rinsing gives you the best protection.

What Doesn’t Work (And Why)
Some people think using a spacer means they can skip rinsing. That’s a myth. A 2024 study in the European Respiratory Journal found that even with a spacer, 30% of patients still had oral deposits. Spacers reduce the amount of medicine in your mouth-they don’t eliminate it. That’s why the American Academy of Allergy, Asthma & Immunology still recommends rinsing after every use, spacer or not.
Another misconception: mouthwash is better than water. It’s not. Alcohol-based mouthwashes can dry out your mouth, which makes thrush worse. Saliva is your body’s natural defense. Dry mouth = more yeast growth. Stick to plain water. If you want extra protection, some studies suggest probiotic rinses may help-but they’re not necessary for most people.
Who’s at Highest Risk?
Not everyone gets thrush or hoarseness. But some people are much more likely to.
- Those taking high doses-above 800 mcg per day of beclomethasone equivalent (like 500 mcg of fluticasone twice daily).
- People with diabetes, especially if HbA1c is above 7.0%. High sugar levels feed yeast.
- Elderly patients. Saliva production drops with age, making it harder to wash away medication.
- Anyone with poor oral hygiene. Brushing twice a day and flossing helps keep your mouth’s natural defenses strong.
If you fall into one of these groups, rinsing isn’t optional. It’s essential.
What to Do If You Already Have Thrush
Don’t panic. Oral thrush is easy to treat. Your doctor can prescribe nystatin oral suspension (a liquid you swish and swallow) or clotrimazole troches (lozenges that dissolve in your mouth). Treatment usually takes 7-14 days. But here’s the catch: if you don’t fix your inhaler routine, it comes back. And it often does. One study found that 40% of patients who treated thrush without changing their habits had it return within a month.
And while you’re treating it, keep using your inhaler. Stopping it could trigger an asthma attack. Just keep rinsing. Even if your mouth is sore, rinse after every puff. Your lungs need the medicine more than your mouth needs to be comfortable.
Practical Tips That Actually Help
Here’s what works in real life:
- Keep water by your bed. If you use your inhaler at night, you’re more likely to skip rinsing because you’re tired. Put a cup of water on your nightstand. Make it part of your routine-like brushing your teeth.
- Clean your spacer weekly. Soap and water. Let it air dry. Don’t wipe it with a towel-fibers can trap medicine. A dirty spacer can become a breeding ground for yeast.
- Check your mouth once a week. Use a flashlight. Look for white patches on your tongue, cheeks, or throat. Early detection means early treatment.
- Ask your doctor or pharmacist to watch you use your inhaler. Studies show that after one 10-minute session with a respiratory therapist, patients reduce oral deposition by 50%. Most people think they’re using it right. They’re not.
- Don’t brush your teeth right after rinsing. Wait 30 minutes. Brushing too soon can remove the protective layer your saliva builds up.
The Bigger Picture
Over 260 million people worldwide use inhaled corticosteroids. That’s a lot of mouths exposed to steroid residue. The global asthma market is growing fast-projected to hit $21.7 billion by 2028. And with more people using these drugs, more are getting thrush and hoarseness. But here’s the good news: we’ve known how to prevent this for over 20 years. The problem isn’t lack of knowledge. It’s lack of action.
A 2023 study found only 45% of patients rinse after every use. That’s not because they don’t care. It’s because no one told them how simple it is. Or they thought it didn’t matter. It does. Every time you rinse, you’re not just protecting your mouth-you’re protecting your ability to breathe without fear.
Some companies are working on better inhalers-ones with built-in spacers or formulas that stick less to your throat. But those won’t be everywhere for years. Right now, the best technology is water, a spacer, and a habit you build in 30 seconds.
Can I use mouthwash instead of water after my inhaler?
No, avoid alcohol-based mouthwashes. They dry out your mouth, which makes oral thrush more likely. Plain water is just as effective and safer. If you want to add something extra, a probiotic rinse may help, but it’s not necessary. Stick to water unless your doctor says otherwise.
Do I need to rinse even if I use a spacer?
Yes. Spacers reduce the amount of medicine that lands in your mouth, but they don’t remove it all. Studies show that even with a spacer, some residue stays behind. Rinsing after using a spacer cuts your risk of thrush and hoarseness even further. The safest approach is to use both-spacer and rinse.
How long does hoarseness last after using an inhaler?
Hoarseness usually lasts a few hours-often 2 to 6 hours-after inhaler use. It’s caused by direct irritation of the vocal cords. If it lasts longer than a day, or if you lose your voice completely, talk to your doctor. It could mean you’re using too high a dose, or there’s another issue like acid reflux. Tilting your head slightly downward when inhaling can reduce vocal cord exposure and help.
Can oral thrush from inhalers be serious?
For most people, it’s uncomfortable but not dangerous. But for those with weakened immune systems-like people with diabetes, HIV, or those on long-term steroids-it can spread to the esophagus and cause swallowing problems. In rare cases, it can become systemic. That’s why early treatment and prevention matter. Don’t ignore white patches. Get them checked.
Will switching inhalers help with hoarseness or thrush?
Some inhalers have lower oral deposition than others. Ciclesonide and mometasone are designed to be less likely to stick in the mouth. But switching alone won’t fix the problem if your technique is wrong. The biggest factor is how you use it-not which brand. Rinsing and using a spacer matter more than the medication itself.
Is it safe to stop using my inhaler if I keep getting thrush?
No. Stopping your inhaler can lead to uncontrolled asthma or COPD flare-ups, which are far more dangerous than thrush. Instead of stopping, fix your routine. Rinse, use a spacer, and talk to your doctor. There’s almost always a way to manage the side effects without giving up the medication.
Final Thought
You didn’t start using an inhaler to get a fungal infection or lose your voice. You started to breathe better. The side effects aren’t inevitable. They’re preventable. It takes 30 seconds after each puff. That’s less time than it takes to check your phone. Do it every time. Your mouth-and your lungs-will thank you.


April Williams
January 27, 2026 AT 14:17You people are so lazy it's disgusting. You'd rather risk your lungs than spend 30 seconds spitting out water? This isn't rocket science. I had thrush for three weeks because my cousin didn't rinse-now she's on antifungals and still can't sing in the choir. Stop making excuses. Rinse. Or don't. But don't act surprised when your mouth turns into a yeast farm.
Kirstin Santiago
January 28, 2026 AT 21:15I used to skip rinsing because I thought it was overkill. Then I got hoarse every morning and wondered why my voice sounded like a rusty hinge. Started rinsing after every puff-no more crackling. It's not glamorous, but it works. Also, my spacer gets a quick rinse once a week. Simple, cheap, and it keeps me breathing. You don't need fancy stuff. Just consistency.
Kathy McDaniel
January 30, 2026 AT 08:01OMG I just realized I never rinsed after my night puff 😳 I’ve been using my inhaler before bed for years and never thought about it… I’m gonna put a cup of water on my nightstand tonight. Fingers crossed no thrush! 🙏
Paul Taylor
January 31, 2026 AT 07:33People keep talking about spacers and rinsing like it’s some new breakthrough but it’s been standard since the 90s. The real issue is that doctors don’t demonstrate proper technique. I had a 10 minute session with a respiratory therapist and suddenly I stopped getting hoarse. Turns out I was inhaling too fast and not holding my breath. No magic pills. No new inhalers. Just learning how to use what you already have. Why is that so hard to get across?
Also the idea that mouthwash is better? That’s like using rubbing alcohol to clean a wound. Dry mouth invites yeast. Water is the only thing you need. And yes, even with a spacer. The residue is still there. You’re not doing yourself any favors pretending otherwise.
Desaundrea Morton-Pusey
February 1, 2026 AT 12:37Why are we letting Big Pharma get away with this? These inhalers are designed to leave residue so you need more meds later. They know people won’t rinse. They know hoarseness makes you feel like it’s not working so you might buy another one. And now they’re pushing expensive spacers like they’re essential. Water costs nothing. Why not just reformulate the damn drug? This whole thing feels like a scam.
Murphy Game
February 3, 2026 AT 03:47Ever wonder why they never tell you this stuff in the pamphlet? Because if you knew how easy it was to avoid side effects, you’d stop blaming the medicine and start blaming the system. They want you dependent. Thrush? Hoarseness? That’s not a side effect-that’s a control mechanism. You think your doctor cares? They get paid per prescription. Rinse? Use a spacer? That’s not in their KPIs. Wake up.
John O'Brien
February 4, 2026 AT 17:35Y’all are overcomplicating this. I’m a mechanic. I don’t have time for fluff. I use my inhaler at work. I spit water into a cup after each puff. Done. No spacer, no probiotics, no drama. Just water. My voice hasn’t cracked in 2 years. My mouth is clean. My asthma is under control. It’s not about being perfect. It’s about being consistent. If I can do it between oil changes, you can do it between scrolling TikTok.
Kegan Powell
February 5, 2026 AT 10:49It’s wild how something so small-30 seconds of rinsing-can change your whole relationship with your health
Most of us think medicine is about pills and devices but really it’s about habits. The inhaler doesn’t work unless you do your part. And that part isn’t hard. It’s just… boring. We want quick fixes but real health is built in quiet moments. Water in the cup. Spitting. Cleaning the spacer. Looking in the mirror once a week. These aren’t chores-they’re rituals. They’re how you say I still care about my body even when I’m tired even when it’s inconvenient even when no one is watching
And if you’ve got thrush? Don’t panic. Don’t stop your inhaler. Just rinse harder. Your lungs are still counting on you. 💪💧