Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t accidents-they’re preventable. You might think, "I’m just taking what the doctor prescribed," but that’s not enough. Medication safety isn’t just about getting the right pill. It’s about knowing when, how, and why you’re taking it-and what to watch out for.
Why Medication Safety Matters More Than You Think
Think of your medications like tools. A hammer won’t work if you try to use it as a screwdriver. The same goes for pills. Take insulin when you don’t need it? Your blood sugar can crash. Skip doses of antibiotics? The infection comes back stronger. Mix warfarin with certain supplements? You could bleed internally. The World Health Organization calls this "Medication Without Harm"-a global push to cut preventable harm by half. In hospitals alone, medication errors contribute to about 7,000 deaths a year in the U.S. That’s not a statistic-it’s someone’s parent, sibling, or neighbor. And it’s not just hospitals. Most errors happen at home, where no one’s watching.The 5 Rights of Safe Medication Use
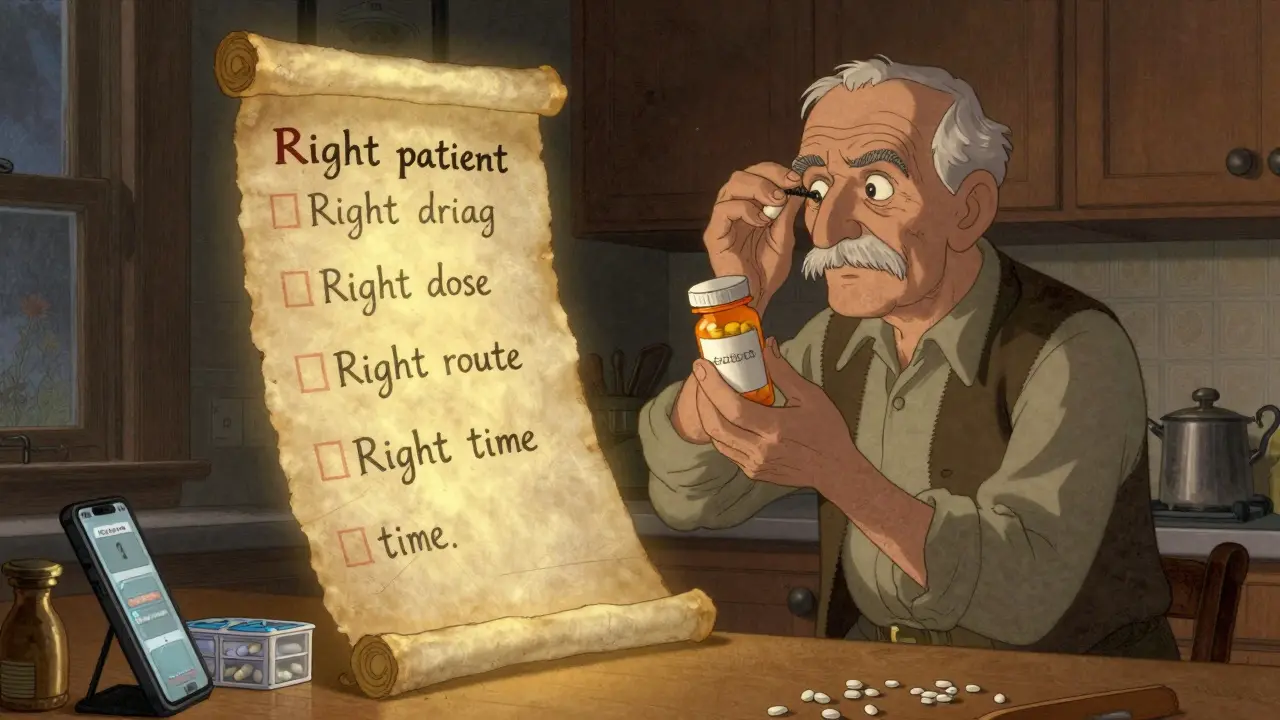
Healthcare professionals use a simple rule called the "Five Rights" to avoid mistakes. You should use it too:- Right patient - Is this medicine really for you? Double-check the name on the bottle.
- Right drug - Does the pill look the same as last time? If it’s a different color or shape, ask your pharmacist.
- Right dose - Is it 5 mg or 50 mg? Don’t guess. Read the label.
- Right route - Is it meant to be swallowed, injected, or applied to the skin? Swallowing a patch won’t help.
- Right time - Taking a pill at night that’s meant for morning can throw off your whole system.
Know Your Medications Like Your Phone Passcode
How many prescriptions do you take? Five? Ten? If you can’t name them all, you’re at risk. The CDC says 50% of medication errors happen during care transitions-like leaving the hospital or switching doctors. Why? Because no one has the full picture. Start a simple list. Write down:- Drug name (brand and generic)
- Dose (e.g., 10 mg)
- How often (e.g., once daily at breakfast)
- Why you take it (e.g., "for high blood pressure")
- Any supplements or over-the-counter drugs (even fish oil or vitamin D)
Ask the FDA’s 8 Questions Before You Take Anything
Your doctor might not have time to explain everything. Don’t wait for them to volunteer details. Ask these questions:- What’s the name of this medicine?
- What’s the active ingredient?
- Why am I taking it?
- How much should I take, and when?
- What should it look like? (Compare to previous refills)
- When does it expire?
- What side effects should I watch for?
- What foods, drinks, or other meds should I avoid?
- What if I miss a dose?
Watch Out for High-Risk Medications
Some drugs are more dangerous than others. The Institute for Safe Medication Practices (ISMP) calls them "high-alert medications." Even a small mistake can be deadly. These include:- Insulin
- Warfarin (blood thinner)
- Heparin (another blood thinner)
- Intravenous oxytocin (used in labor)
Don’t Let Look-Alike, Sound-Alike Drugs Trick You
Glimepiride and glyburide. Prednisone and prednisolone. These names look and sound almost identical. But they’re not the same. One treats type 2 diabetes. The other reduces inflammation. Take the wrong one, and you could end up with dangerously low blood sugar-or a flare-up of your condition. Pharmacies use "Tall Man Lettering" to help: predniSONE vs. predniSOLONE. The capital letters highlight the difference. You can do the same. When you get a new prescription, write the name in your own way-underline the key letters. Add a note: "This is for my arthritis, not my diabetes." Reddit users share stories like this: "Took the wrong pill for three days. Blood sugar crashed. Thought I was dying. Turned out I confused the two diabetes meds." That’s not rare. It’s common.Use Tools That Actually Help
You don’t need fancy gadgets. Simple tools work:- Pill organizers - Use them. Studies show they cut errors by 35% in older adults.
- Smartphone alarms - Set one for each dose. Label it: "Take blood pressure pill-7 AM".
- Medication apps - The CDC launched a free checklist app in January 2024. It lets you scan your pills, track doses, and get alerts.
- One pharmacy only - Fill all your prescriptions at the same place. That way, the pharmacist sees everything you’re taking and can catch dangerous interactions.
Never Stop or Skip Doses Without Talking to Someone
You feel better. So you stop the antibiotics. You’re tired of the side effects, so you skip the antidepressant. You think, "I don’t need this anymore." That’s dangerous. The FDA says 23% of antibiotic failures happen because people stop early. The infection doesn’t die-it mutates. Now it’s stronger. And harder to treat. Antidepressants? Stopping suddenly can cause withdrawal symptoms: dizziness, nausea, even seizures. Always talk to your doctor first. They might suggest tapering slowly.

Bryan Coleman
February 1, 2026 AT 06:18Just got back from the pharmacy and realized I’ve been taking my blood pressure med at night instead of morning. Holy crap. I’m setting alarms now. Thanks for the reminder.
Also, my pharmacist caught that I was mixing turmeric with warfarin. Dude saved my life. Pharmacists are unsung heroes.
Naresh L
February 1, 2026 AT 20:49It’s funny how we treat our bodies like machines that run on invisible code. We don’t question the firmware updates, but we’ll argue with a doctor over a pill. Maybe safety isn’t about rules-it’s about humility. We’re not in control. The body is. We just borrow it.
Sami Sahil
February 3, 2026 AT 00:59YESSSS! I used to skip my meds when I felt fine. Then I ended up in the ER with a heart palpitation nightmare. Now I’ve got my pill organizer, alarms, and a sticky note on my mirror that says ‘DON’T BE A DUMBASS.’ Works like a charm. You got this!
franklin hillary
February 3, 2026 AT 05:23Look I’ve been doing this for 20 years and I can tell you the system is broken. Doctors don’t have time. Pharmacies are understaffed. Patients are distracted. But here’s the truth nobody wants to admit-medication safety isn’t about checklists. It’s about power. The pharmaceutical industry doesn’t want you to know how dangerous these drugs are. They want you dependent. They profit from your confusion. I’ve seen it. I’ve lived it. And I’m not just talking about insulin or warfarin. I’m talking about the entire structure. The FDA is a revolving door. The pills you take are designed to keep you coming back. You think you’re in control? You’re a customer.
Wake up. Read the labels. Question everything. Even the advice in this post. Because someone’s making money off your compliance.
Jaden Green
February 3, 2026 AT 22:25Let’s be honest-this post reads like a public service announcement written by a hospital marketing intern. Five Rights? Really? That’s the gold standard? I’ve worked in clinical research. The real problem is polypharmacy in the elderly, lack of pharmacogenomic testing, and the fact that 80% of prescriptions are written without proper drug interaction screening. You’re telling people to write things down on sticky notes while the system is actively failing them. This is like handing someone a flashlight in a hurricane and calling it safety.
Lu Gao
February 4, 2026 AT 12:14OMG I just realized I’ve been taking my thyroid med with coffee for 3 years 😱 I thought it was fine because my doctor didn’t say anything. Now I’m gonna drink my coffee 30 mins AFTER the pill. Also, why is everyone ignoring the fact that the CDC app is literally called ‘Medication Safety Check’? I’ve been using it since January. It’s free. It’s easy. Why are we still doing this the hard way? 🙄
Angel Fitzpatrick
February 4, 2026 AT 21:50They don’t want you to know this but insulin isn’t just for diabetes. It’s a growth hormone. The FDA and Big Pharma are pushing it because it keeps people on lifelong dependency. Same with warfarin-there are natural alternatives like nattokinase that they bury because they can’t patent them. You think your pharmacist is helping you? They’re paid by the pharmaceutical reps. The ‘Five Rights’? A distraction. The real issue is the medical-industrial complex. Your pills are designed to make you sick enough to need more pills. Wake up. Read the ingredients. Look for fillers like magnesium stearate-those are immunosuppressants. You’re being poisoned slowly. And they call it ‘treatment’.
Melissa Melville
February 5, 2026 AT 07:18So… we’re supposed to be this proactive about meds but no one taught us how? Like, my grandma took six pills a day and thought ‘if it’s prescribed, it’s safe.’ She died from a bleeding ulcer caused by mixing aspirin and ibuprofen. And now we’re all supposed to be pharmacists? Cool. I’ll just start carrying a clipboard and a magnifying glass to Target.
Naomi Walsh
February 5, 2026 AT 08:23How quaint. A list of basic hygiene practices presented as revolutionary insight. In Europe, we’ve had mandatory medication reconciliation protocols since 2012. We use electronic prescribing with AI-driven interaction alerts. We don’t rely on elderly patients writing notes on napkins. This post reads like a 1998 pamphlet. If you’re still using pill organizers and alarms, you’re already behind the curve. The future is blockchain-based medication tracking and AI-assisted adherence monitoring. Until then, you’re just bandaging a ruptured artery.
Bob Cohen
February 6, 2026 AT 08:07Man, I used to think I was fine until my mom had a near-fatal interaction between her blood thinner and a new herbal tea she started taking. She didn’t even think it was a drug. Now we all have a shared Google Doc with every pill, supplement, and ‘natural remedy’ we take. It’s not glamorous. But it works. And honestly? Talking to your pharmacist feels like asking a friend for advice-not a sales pitch. They’re the real MVPs.
Nancy Nino
February 7, 2026 AT 16:55It is imperative to underscore the gravity of non-adherence to prescribed pharmacological regimens, as elucidated within this comprehensive exposition. The statistical prevalence of preventable adverse drug events is not merely an epidemiological concern-it is a moral imperative for patient autonomy and systemic accountability. One must, therefore, engage in rigorous documentation, temporal precision, and pharmacovigilant vigilance at all junctures of therapeutic intervention.
June Richards
February 9, 2026 AT 09:14LOL at the CDC app. I downloaded it. It asked me to scan my pills. My bottle had a QR code that linked to a 2017 website that doesn’t exist anymore. Then it asked me to manually type in the name of my antidepressant. I typed ‘sertraline’. It said ‘invalid drug’. I gave up. Now I just use a sticky note and a prayer. 😂