Hot flashes that wake you up at 3 a.m. Night sweats so bad you need a change of pajamas. Mood swings that leave you wondering if you’re still you. For millions of women, these aren’t just inconveniences-they’re life-altering. If you’re in your late 40s or early 50s and struggling with menopause symptoms, you’ve probably heard about hormone therapy. But should you try it? Is it safe? And if so, which kind?
What Is Hormone Therapy for Menopause?
Menopause hormone therapy (MHT), often called hormone replacement therapy or HRT, is the use of estrogen, sometimes with progestogen, to ease symptoms caused by the drop in hormones during menopause. It’s not a cure. It’s not a magic pill. But for many women, it’s the most effective tool we have for managing severe hot flashes, night sweats, and vaginal dryness.
Estrogen is the main hormone used. It comes in different forms: pills, patches, gels, sprays, and vaginal creams or rings. If you still have a uterus, you’ll also need progestogen to protect against uterine cancer. Without it, estrogen alone can cause the lining of the uterus to thicken-raising cancer risk.
There are two main types: estrogen-only therapy (for women who’ve had a hysterectomy) and combined estrogen-progestogen therapy (for those with a uterus). The dose matters too. The lowest amount that works is what doctors now recommend. High doses? Outdated. Low doses? Standard.
Why Do Women Use It?
The biggest reason? Relief. Severe hot flashes can happen 15 to 20 times a day. That’s exhausting. That’s isolating. That’s embarrassing. Studies show hormone therapy reduces hot flashes by 75% or more-far better than anything else.
Compare that to non-hormonal options. SSRIs like fluoxetine might cut hot flashes by 50-60%. Gabapentin? Around 45%. Plant-based remedies like soy or black cohosh? A Cochrane Review found they’re barely better than a placebo-maybe half a fewer hot flash per day.
It’s not just about comfort. MHT also helps preserve bone density. After menopause, bone loss speeds up. A woman can lose up to 20% of her bone mass in the first five years. Hormone therapy slows that down. For women at high risk of osteoporosis, it’s a proven shield.
And then there’s vaginal health. Estrogen creams or rings restore moisture, reduce pain during sex, and prevent recurrent urinary infections. These aren’t minor issues-they affect relationships, confidence, and quality of life.
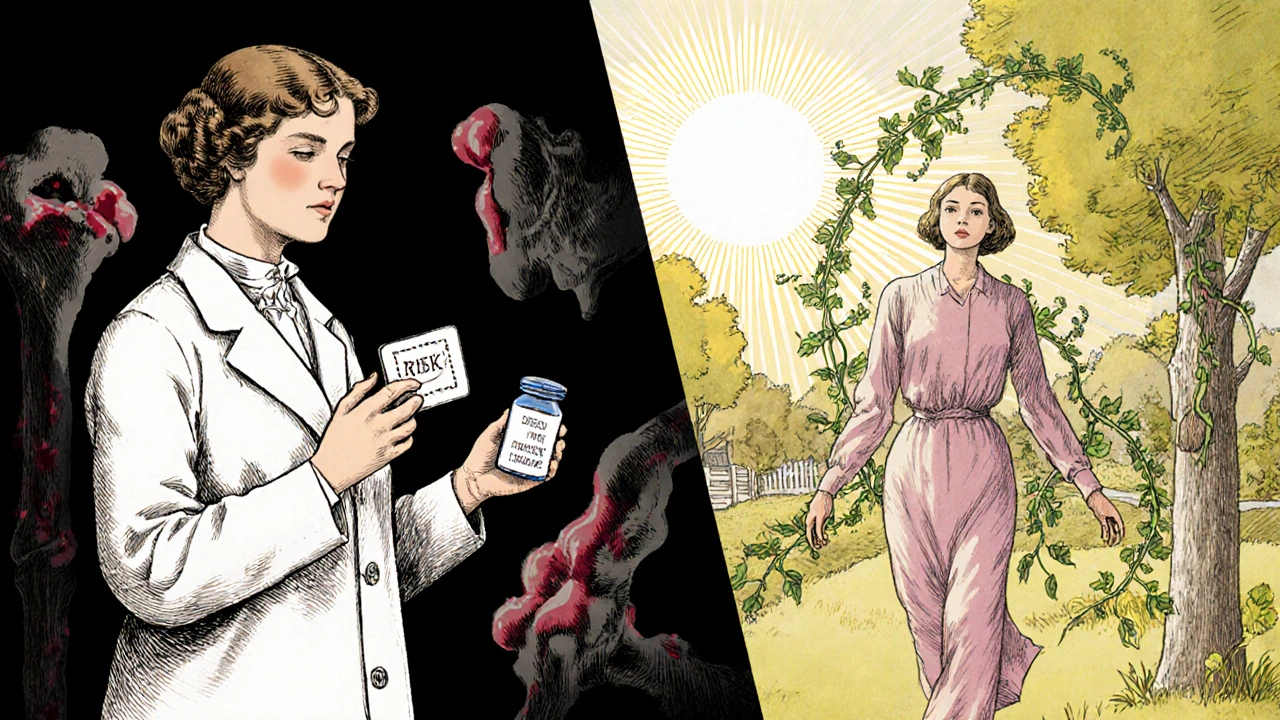
What Are the Real Risks?
Here’s where things get complicated. The fear around hormone therapy started in 2002, after the Women’s Health Initiative study linked it to increased risks of breast cancer, heart disease, stroke, and blood clots. That study changed everything. Millions of women stopped taking it. Prescriptions dropped by 70%.
But here’s what most people don’t know: those risks weren’t the same for everyone. They depended on age, timing, and formulation.
For women under 60 or within 10 years of menopause onset, the benefits usually outweigh the risks. For women starting therapy after 60-or more than 10 years past menopause-the risks go up. That’s the “timing hypothesis,” and it’s now backed by decades of data.
Let’s break it down:
- Breast cancer: Combined therapy increases risk by about 29 extra cases per 10,000 women per year. Estrogen-only? No significant increase-just 9 extra cases. And the risk rises with longer use. After 5 years, the increase becomes more noticeable.
- Blood clots: Oral estrogen increases risk of venous thromboembolism (VTE) by 3 times compared to placebo. Transdermal (patch or gel) estrogen? Only 1.3 times higher. That’s why many doctors now prefer patches over pills.
- Stroke: Oral estrogen raises stroke risk by about 30%. Transdermal doesn’t. If you have high blood pressure or other stroke risk factors, this matters.
- Heart disease: In women starting therapy after 60, there’s a slight increase in heart attack risk in the first year. But for women under 60, the risk is neutral-or even slightly protective.
And here’s something important: not all progestogens are equal. Micronized progesterone (natural, body-identical) has a better safety profile than medroxyprogesterone acetate (synthetic). The latter is linked to higher breast cancer risk.
Which Formulation Is Best?
Not all hormone therapies are created equal. The delivery method changes everything.
Oral estrogen (pills) passes through the liver first. That triggers changes in clotting factors and inflammation markers. That’s why it raises blood clot and stroke risk more than other forms.
Transdermal estrogen (patches, gels, sprays) enters the bloodstream directly. No liver first pass. That means lower VTE risk-about 50% less than pills. It’s also more stable, with fewer spikes and crashes in hormone levels.
For women with hot flashes, patches like Estraderm or gels like EstroGel are often preferred. For vaginal symptoms, low-dose vaginal estrogen (tablets, rings, creams) works locally with almost no systemic absorption. That means almost no risk to the rest of your body.
And cost? Generic estradiol pills cost $15-$30 a month. Brand-name patches? $150-$250. Insurance often covers generics. Ask your doctor.
Who Should Avoid It?
Hormone therapy isn’t for everyone. Absolute contraindications include:
- History of breast cancer
- History of blood clots (DVT or pulmonary embolism)
- History of stroke or heart attack
- Unexplained vaginal bleeding
- Active liver disease
- Known estrogen-sensitive cancers
If you have a family history of breast cancer or clotting disorders, talk to your doctor. Genetic testing isn’t routine yet-but it’s coming. Some clinics now offer metabolic profiling to see how your body processes estrogen. That could help personalize therapy in the next few years.
And if you’re over 65? Most experts say the risks outweigh the benefits for symptom relief. But if you’re 62 and still having severe hot flashes? That’s a different conversation.
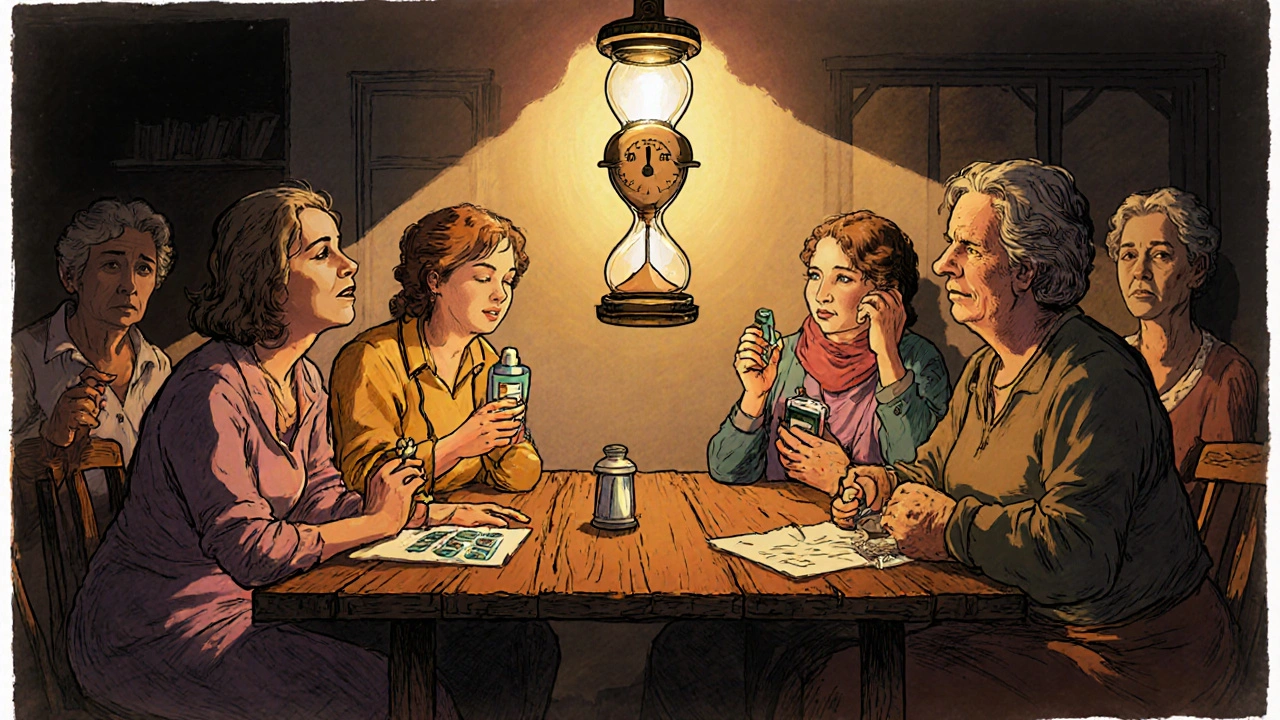
What Do Real Women Say?
On forums like Reddit’s r/menopause and Menopause Matters, stories vary wildly.
“I went from 20 hot flashes a day to 2 or 3 in 10 days on a 0.05 mg estradiol patch,” wrote one user in March 2024.
Another: “I quit after three months because of bloating and mood swings. It felt like I was on a rollercoaster.”
A 2023 survey found that 72% of women who stopped hormone therapy did so because of fear of breast cancer. Only 18% cited side effects. That tells you something: fear often outweighs experience.
And then there’s the long-term users. “My DEXA scan after 8 years on HRT showed stable bone density,” one woman wrote in January 2025. “My sister, who refused HRT, broke her hip at 62.”
These aren’t anecdotes. They’re real people making real choices based on real results.
How Do You Start?
It’s not a decision you make alone. Talk to your doctor. Bring your symptoms. Bring your fears. Bring your family history.
Here’s what a good first visit looks like:
- Review your symptoms using a scale like the Menopause Rating Scale.
- Check your blood pressure and weight.
- Discuss your personal and family history of cancer, clots, heart disease.
- Decide on the lowest effective dose.
- Choose transdermal over oral if you have any risk factors.
- Start with micronized progesterone if you still have a uterus.
Breakthrough bleeding is common in the first 3-6 months. Don’t panic. It usually settles. If it doesn’t, your dose may need adjusting.
Most women start feeling better in 2-4 weeks. Give it time. Track your symptoms. If you don’t see improvement after 8 weeks, it’s not working. Try a different form or dose.
How Long Should You Stay on It?
There’s no hard deadline. But the rule is: use it for the shortest time needed to manage symptoms.
For most women, that’s 3-5 years. Some need it longer-for bone health, for quality of life, for sleep. If you’re under 60 and doing well, continuing beyond 5 years is often safe.
Reassess every year. Ask: Are my symptoms still bad? Do I still need it? Are my risks changing? Your body changes. So should your plan.
Stopping? Don’t quit cold turkey. Gradual tapering reduces rebound hot flashes. Talk to your doctor about a plan.
What’s New in 2025?
The conversation around hormone therapy is shifting again. In July 2025, an FDA expert panel reviewed over 120 million patient records and confirmed what many doctors have been saying: starting estrogen during perimenopause lowers heart disease risk by 18% compared to starting after menopause.
That’s huge. It means the window of opportunity isn’t just 10 years after menopause-it might start before it even ends.
Also new: the 2025 Endocrine Society guidelines are expected to formally define this “window of opportunity” with specific age cutoffs. And yes, genetic testing to tailor estrogen metabolism is on the horizon.
Meanwhile, more employers are stepping in. Over 40% of Fortune 500 companies now offer menopause support programs. That’s not just HR-it’s recognition that this isn’t a personal issue. It’s a workplace issue.
Final Thoughts
Hormone therapy isn’t right for every woman. But it’s not the dangerous, one-size-fits-all treatment it was painted to be in the 2000s. The science has evolved. So should the conversation.
If you’re under 60 and struggling with menopause symptoms, don’t assume you have to suffer. Don’t assume hormone therapy is too risky. Ask questions. Get informed. Talk to a specialist-look up a NAMS-certified provider. There are over 1,850 in the U.S. alone.
The goal isn’t to take hormones forever. It’s to get through this transition with your health, your comfort, and your dignity intact.


Leisha Haynes
November 25, 2025 AT 03:50My hot flashes went from 15 a day to 2 after starting a 0.05mg patch
Why are we still pretending natural remedies work when the science says otherwise?
Kimberley Chronicle
November 25, 2025 AT 13:24Starting HRT within 10 years of menopause onset isn't just safer-it's cardioprotective
Yet most primary care docs still treat it like a 2002 relic
We need better education, not fear-mongering
Also-transdermal over oral, always. The hepatic first-pass effect is why pills carry higher VTE risk
giselle kate
November 25, 2025 AT 20:51Meanwhile, women in Europe get bioidentical hormones without a fight
Why do we treat menopause like a moral failing instead of a physiological transition?
It's not just about estrogen-it's about respect
And if you're still scared of breast cancer, get your BRCA tested instead of punishing yourself with hot flashes
Lisa Odence
November 26, 2025 AT 12:35Shirou Spade
November 27, 2025 AT 18:42We treat it like a glitch in a woman's system rather than a natural phase
But the real tragedy isn't the symptoms-it's that we've made women feel guilty for wanting to feel normal again
Estrogen isn't a drug
It's a return to balance
Dolapo Eniola
November 28, 2025 AT 12:28Big Pharma pushed this for decades
They made billions off estrogen pills while hiding the risks
Now they're rebranding it as 'safe' because they want more profit
Why are you trusting doctors who got their info from pharmaceutical reps?
Try yoga. Try acupuncture. Try not eating dairy
Real healing isn't in a pill
Josh Zubkoff
November 30, 2025 AT 03:52The 2002 WHI study didn't lie
They just didn't break down the data by age and route
Now they're cherry-picking the 2025 meta-analysis like it's gospel
Meanwhile, my cousin got a blood clot on a patch
And now she's on warfarin for life
So no, I'm not 'scared'-I'm informed
And I'm not your guinea pig
fiona collins
December 1, 2025 AT 19:07Rachel Villegas
December 1, 2025 AT 23:14Andrew Camacho
December 3, 2025 AT 00:30But the truth is, doctors have known this for years
They just didn't want to fight the media storm
Now that the narrative has shifted, suddenly everyone's a HRT advocate
Meanwhile, women who tried it in 2003 and had bad outcomes? Forgotten
It's not about science-it's about who's telling the story right now
Arup Kuri
December 3, 2025 AT 10:43Why is the hormone we're born with the villain?
Big Pharma wants you scared
They sell you antidepressants for hot flashes
They sell you sleep aids for night sweats
But they don't sell you the truth-your body just needs its own estrogen back
Elise Lakey
December 4, 2025 AT 17:46Karen Willie
December 5, 2025 AT 01:29Erika Hunt
December 6, 2025 AT 01:38For decades, we've been told to 'tough it out' or 'it's just aging'
But menopause isn't a weakness-it's a biological pivot
And if we had treated it like heart disease or diabetes-with urgency, funding, and research-we wouldn't be having this conversation in 2025
It's not just about estrogen-it's about valuing women's health beyond fertility
prasad gaude
December 7, 2025 AT 14:33Women take ashwagandha, shatavari, and coconut oil
They don't go to doctors-they go to grandmothers
But here's the truth: some of us need more than herbs
Some of us need science
And that doesn't make us less Indian or less spiritual
It makes us human
Timothy Sadleir
December 8, 2025 AT 10:09Ellen Sales
December 8, 2025 AT 19:11Andrew McAfee
December 9, 2025 AT 18:30She started patches, got her bone density back, started sleeping again
Now she's hiking again
And I'm just glad we found the right path
Menopause isn't a women's issue
It's a family issue