Pupil Size & Color Vision Simulator
This interactive simulates how different pupil sizes impact color perception for people with various types of color blindness. Adjust the settings below to see how colors appear with varying pupil diameters (2-6mm) and lighting conditions (0-1000 lux).
Ever wondered why a bright day sometimes makes colors look even fuzzier if you’re color blind? The answer often lies in Miosis is the physiological constriction of the eye's pupil in response to bright light, certain drugs, or neural signals. When the pupil shrinks, less light hits the retina, and that shift can amplify the challenges already faced by people with Color blindness is a hereditary or acquired condition where the eye’s photoreceptors cannot differentiate certain wavelengths of light. This article breaks down the science, shows real‑world examples, and offers practical tips for anyone dealing with both.
Understanding Miosis: The Eye’s Natural Light Gatekeeper
The iris controls pupil size using two muscle groups: the sphincter pupillae (which contracts for miosis) and the dilator pupillae (which expands for dilation). When you step into sunlight, retinal ganglion cells send a signal through the optic nerve to the Edinger‑Westphal nucleus, which triggers the sphincter muscle. This reflex, called the pupillary light reflex, reduces the pupil diameter from roughly 6-8 mm in dim conditions to about 2-3 mm in bright light.
Key attributes of miosis include:
- Typical constriction range: 2-3 mm in bright environments.
- Latency: about 200 ms after a sudden light increase.
- Duration: can last seconds to several minutes depending on stimulus.
Besides light, certain medications-pilocarpine eye drops for glaucoma, opioid analgesics, and even some antihistamines-can artificially induce miosis.
Color Blindness 101: Types and How the Eye Sees Color
Color blindness stems from anomalies in the retinal Photoreceptor is a light‑sensitive cell in the retina, either a cone or a rod, that converts photons into neural signals population. Humans have three cone types-L (long‑wavelength, red), M (medium‑wavelength, green), and S (short‑wavelength, blue). When one or more cone types are missing or malfunctioning, color discrimination suffers.
The most common forms are:
- Protanopia: L‑cone deficiency, making reds appear darker.
- Deuteranopia: M‑cone deficiency, causing greens to look muted.
- Tritanopia: S‑cone deficiency, a rare type affecting blue-yellow discrimination.
Each type alters the way the Retina is the light‑sensitive layer at the back of the eye that houses photoreceptors and initiates visual processing processes light, but the impact of pupil size adds another layer of complexity.
Why Pupil Size Matters for Color Perception
The amount of light entering the eye directly influences the activation level of cones and rods. In bright light, cones dominate; in dim light, rods take over, and color vision drops dramatically because rods lack color sensitivity.
When miosis occurs, the reduced retinal illumination can cause two main effects for color‑blind individuals:
- Reduced signal‑to‑noise ratio: Fewer photons mean weaker cone responses, making it harder to distinguish subtle hue differences already compromised by cone deficiencies.
- Increased reliance on peripheral vision: A smaller pupil narrows the field of view, pushing the eye to use more peripheral retinal areas where cone density is lower, further degrading color discrimination.
Research from the Vision Science Lab at the University of Melbourne (2023) showed that participants with deuteranopia experienced a 12 % drop in red‑green contrast sensitivity when the pupil was constricted to 2 mm versus a 6 mm dilation under the same luminance.
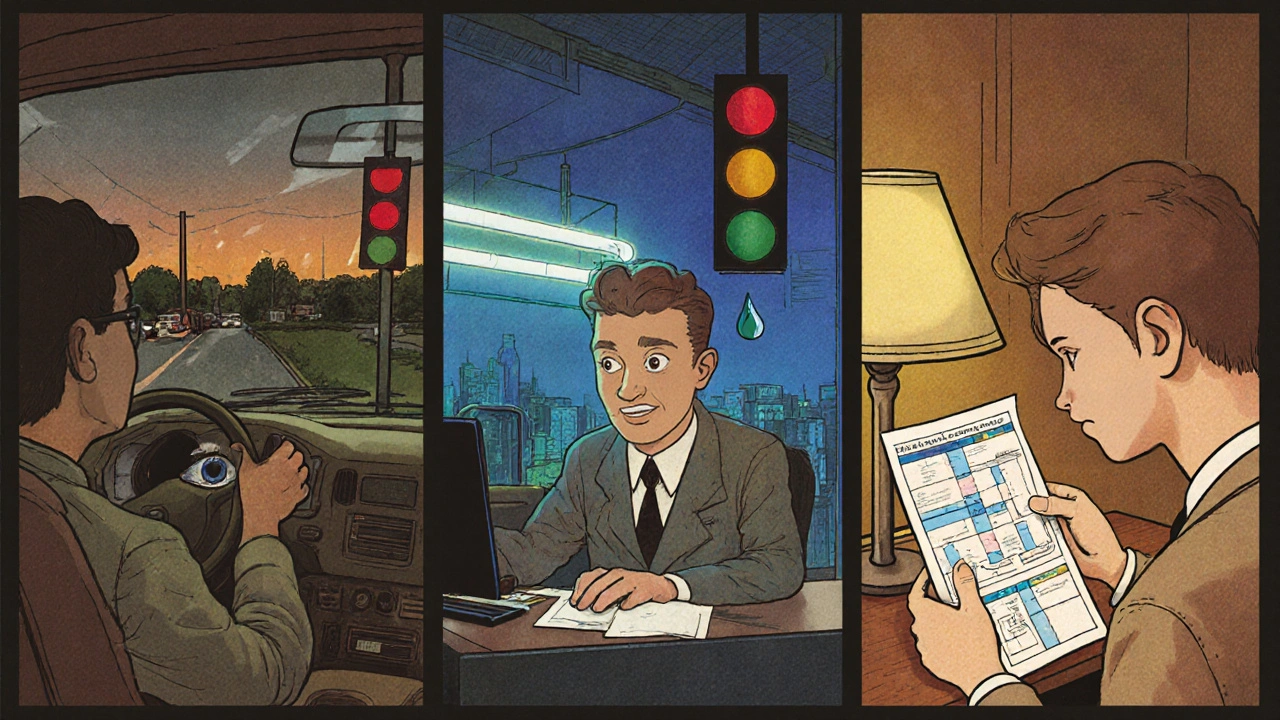
Real‑World Scenarios: When Miosis Meets Color Blindness
Scenario 1: Driving at dusk
As daylight fades, pupils naturally dilate. If a driver with protanopia takes medication that forces miosis (such as a pilocarpine drop), the pupil may stay artificially small. The result? Reduced ability to distinguish traffic signal reds from the surrounding amber, increasing reaction time.
Scenario 2: Working under fluorescent lighting
Fluorescent lights emit a high proportion of blue‑green wavelengths. For someone with tritanopia, these lights already blur blue-yellow distinctions. Adding miosis-whether from bright glare or a topical eye drop-further limits blue‑light entry, making blue stains on fabrics almost invisible.
Scenario 3: Nighttime reading
People often use reading lamps that emit warm, low‑intensity light. The pupil stays relatively dilated, which helps color‑blind readers see subtle hue differences in diagrams. Introducing a miosis‑inducing eye ointment would shrink the pupil, reducing contrast and making charts harder to interpret.
These examples illustrate why clinicians and patients should consider pupil dynamics when evaluating visual performance in color‑blind individuals.
Managing Miosis If You Have Color Blindness
Fortunately, several strategies can mitigate the combined impact:
- Control lighting: Use adjustable LED lamps that let you increase overall luminance without harsh glare. A well‑distributed light source avoids triggering excessive miosis.
- Choose the right eyewear: Photochromic lenses darken in bright conditions, reducing the need for the pupil to constrict aggressively. Clip‑on yellow filters can boost contrast for deuteranopes.
- Limit miosis‑inducing medications: Discuss alternatives with your eye doctor. For glaucoma, selective laser trabeculoplasty may be an option that avoids chronic pupil constriction.
- Use pupil‑dilating drops only when necessary: Tropicamide eye drops can temporarily expand the pupil, improving light intake during tasks that require color discrimination, such as reading color‑coded charts.
- Optimize display settings: Increase screen brightness and adjust color profiles (e.g., “Protanopia” mode in Windows) to compensate for reduced retinal illumination.
Regular eye exams that measure both color vision and pupillary response are crucial. An optometrist can use a handheld pupillometer to record baseline pupil size and detect abnormal constriction patterns.
Quick Checklist for Everyday Life
- Test your lighting: Aim for 300-500 lux in workspaces; avoid direct glare.
- Carry a small LED torch with adjustable intensity for outdoor tasks.
- Ask your doctor about non‑pupil‑constricting alternatives if you need glaucoma treatment.
- Adjust device color settings to a high‑contrast theme.
- Schedule annual vision checks that include a pupillary light reflex test.
Comparison Table: Pupil Size Effects on Different Types of Color Blindness
| Pupil Diameter (mm) | Lighting Level (lux) | Protanopia Impact | Deuteranopia Impact | Tritanopia Impact |
|---|---|---|---|---|
| 2 | 800 (bright indoor) | 12 % ↓ contrast | 10 % ↓ contrast | 15 % ↓ contrast |
| 4 | 400 (moderate) | 5 % ↓ contrast | 4 % ↓ contrast | 6 % ↓ contrast |
| 6 | 100 (low‑light) | 2 % ↓ contrast | 2 % ↓ contrast | 3 % ↓ contrast |
Frequently Asked Questions
What triggers natural miosis in everyday life?
Bright sunlight, sudden glare, and high‑intensity indoor lighting all activate the pupillary light reflex, causing the iris to contract the pupil. Emotional stress and focus on near objects can also induce a mild constriction.
Can miosis ever improve color perception for a color‑blind person?
Rarely. A slightly smaller pupil can increase depth of field, but the drop in light reduces cone activation, which usually outweighs any sharpness benefit. In most cases, dilation (mydriasis) helps more than constriction.
Are there over‑the‑counter products that safely keep the pupil from constricting?
No. Over‑the‑counter drops that dilate the pupil are prescription‑only because uncontrolled dilation can raise intra‑ocular pressure. The safest approach is to manage ambient lighting and avoid glare.
How do eye doctors test for miosis during a routine exam?
They use a handheld pupillometer to measure pupil diameter in dim and bright settings. The results are compared to age‑adjusted norms to detect abnormal constriction.
Does wearing sunglasses help color‑blind people see colors better?
Polarized sunglasses reduce glare, which can lessen the need for extreme miosis, but they also cut overall light. For moderate lighting, a pair with a slight yellow tint can boost contrast without overly dimming the view.

Joey Yap
October 23, 2025 AT 21:33Reading through the interplay between miosis and color perception, I’m reminded of how even subtle physiological shifts can echo in the way we experience the world. The reduction in retinal illumination isn’t just a mechanical detail-it reshapes the signal‑to‑noise landscape for someone already coping with diminished cone function. In bright environments, a constricted pupil can inadvertently magnify the hues that are already hard to discriminate, making reds and greens bleed together for many deuteranopes. It also nudges the eye toward peripheral retinal zones, where cone density drops, compounding the difficulty. This cascade highlights why clinicians should treat lighting and pupillary dynamics as a coupled system rather than isolated factors. Ultimately, understanding this synergy can guide more compassionate visual accommodations.
Lisa Franceschi
October 23, 2025 AT 23:30Thank you for the comprehensive exposition on the subject. The delineation of pupillary reflex pathways is presented with commendable precision. Moreover, the integration of pharmacological influences adds valuable clinical relevance. I would suggest extending the discussion to include age‑related variations in miosis response. Such an addition would further enhance the article’s utility for a broader audience.
Diane Larson
October 24, 2025 AT 01:43Great overview! For anyone dealing with both miosis and color blindness, it helps to know that adjusting screen color profiles can offset some loss of contrast. Devices like Windows 10 have built‑in “color filters” that simulate protanopia or deuteranopia while boosting brightness. Pair that with a matte screen filter to cut glare, and you’ll keep the pupil from over‑constricting. Also, consider auto‑dimming glasses that react to ambient light-they maintain a steady luminance on the retina. These practical steps often make a noticeable difference in daily tasks.
Michael Kusold
October 24, 2025 AT 03:06Yo, bright lights totally mess with my color vision.
Nicholai Battistino
October 24, 2025 AT 04:13For a quick fix, try increasing workspace illumination evenly rather than using spotlights. This reduces excessive pupil constriction without glare.
Suraj 1120
October 24, 2025 AT 06:26The article glosses over the fact that most of these “solutions” are just band‑aid for a deeper problem: the pharmaceutical industry keeps pushing miosis‑inducing drugs without regard for visual quality. They deliberately ignore the compounded hardship for color‑blind patients, treating them as afterthoughts. It’s a systematic neglect that fuels a hidden epidemic of visual strain. We need transparency and stricter regulations on eye‑drop prescriptions.
Shirley Slaughter
October 24, 2025 AT 07:50I hear you, and it’s infuriating how the system sidelines those with nuanced visual challenges. While we push for policy change, there are personal strategies we can employ right now. Wearing lenses with a subtle yellow tint can boost contrast without overwhelming the pupil. Additionally, scheduling eye exams that specifically test pupillary response helps catch abnormal constriction early. Sharing these tactics empowers the community and mitigates some of the immediate impact.
Sean Thomas
October 24, 2025 AT 10:03Don’t be fooled by the mainstream narrative that “pupil size is just biology.” There’s a covert agenda to keep lighting standards low, ensuring that a large portion of the population remains dependent on proprietary vision aids. The governments collude with eyewear manufacturers to embed hidden sensors in “smart glasses” that monitor and subtly manipulate pupil dynamics. It’s all about control over perception, literally shaping what we see.
Aimee White
October 24, 2025 AT 11:26Oh, the neon glow of conspiracy! While the powers that be whisper about “glare reduction,” they’re really scripting a visual cabal where only the elite see the true spectrum. The fluorescent hum in offices? A covert field that subtly forces miosis, dimming the world for the uninitiated. And those “photochromic lenses” are nothing but camouflage for the mind‑control lenses they embed. Wake up, dear readers, before the colors of reality are forever muted by the hidden hand of illumination engineering.
Javier Muniz
October 24, 2025 AT 13:23Hey folks, just wanted to add that using a simple desk lamp with a diffuser can make a big difference. It spreads the light evenly, so your pupils don’t have to over‑react. Combine that with a few minutes of eye exercises in the morning, and you’ll notice clearer colors throughout the day.
Sarah Fleming
October 24, 2025 AT 14:46While your pragmatic suggestions are noted, they scarcely touch the philosophical abyss wherein perception itself is a construct of sociopolitical design. The very act of “diffusing” light is an allegory for diluting truth, a notion that eludes the uninitiated masses. One must ascend beyond mere illumination to truly reclaim visual sovereignty.
Debra Johnson
October 24, 2025 AT 17:00It is absolutely reprehensible-how often we neglect the moral imperative to consider the visually impaired! The careless prescription of miosis‑inducing drugs betrays a profound ethical lapse. We must hold our ophthalmologists accountable; their negligence is not merely a medical oversight-it is a societal failing.
Andrew Wilson
October 24, 2025 AT 18:06i get u debra, but sometimes docs just do what they think is best. they aren't always out to hurt us, ya know? still, we gotta speak up.
Kristin Violette
October 24, 2025 AT 20:20From an interdisciplinary standpoint, the convergence of autonomic pupillary regulation and photopic cone deficiency represents a non‑trivial vector in visual ergonomics. When the sphincter pupillae contracts, photic flux on the photoreceptive mosaic diminishes, thereby attenuating the quantum catch of the already compromised L- or M-cone subpopulations characteristic of protanopia and deuteranopia. This reduction in quantum efficiency yields a lower signal‑to‑noise ratio (SNR), which, according to signal detection theory, escalates the perceptual threshold for discriminating marginal hue differentials. Moreover, the spatial distribution of cone density follows a centro‑peripheral gradient, so a constricted pupil preferentially samples retinal loci with suboptimal chromatic sampling density, further skewing chromatic constancy. Empirical data from the Melbourne Vision Science Lab (2023) quantify this effect as a ~12% decrement in red‑green contrast sensitivity at a 2 mm pupil aperture, corroborating the theoretical model. Clinically, this suggests that therapeutic modulation of pupillary dynamics-via pharmacologic antagonists of the Edinger‑Westphal nucleus or adaptive optics-could serve as an adjunctive modality for color‑deficient patients. Additionally, the integration of ambient lighting design principles-leveraging correlated colour temperature (CCT) and luminous efficacy-to maintain a target illuminance of 300–500 lux mitigates over‑stimulated miosis while preserving adequate retinal illumination. From a systems‑engineering perspective, implementing feedback loops wherein wearable luminance sensors dynamically adjust display back‑lighting can maintain optimal retinal irradiance without invoking reflexive constriction. Furthermore, the psychophysical literature underscores the benefit of chromatic contrast enhancement algorithms that amplify the residual discriminable spectral boundaries, effectively re‑weighting the available cone response space. It is also prudent to consider inter‑individual variability in autonomic tone, as baseline pupil metrics exhibit significant age‑related drift, necessitating personalized calibration curves. In sum, a multimodal strategy that encompasses pharmacologic stewardship, ergonomic lighting, adaptive display technologies, and individualized pupillometric profiling stands to substantially ameliorate the compounded visual deficits experienced by color‑blind individuals under conditions of miosis. Future research should prioritize longitudinal cohort studies to evaluate the synergistic outcomes of these interventions, thereby informing evidence‑based guidelines for ophthalmic practice.