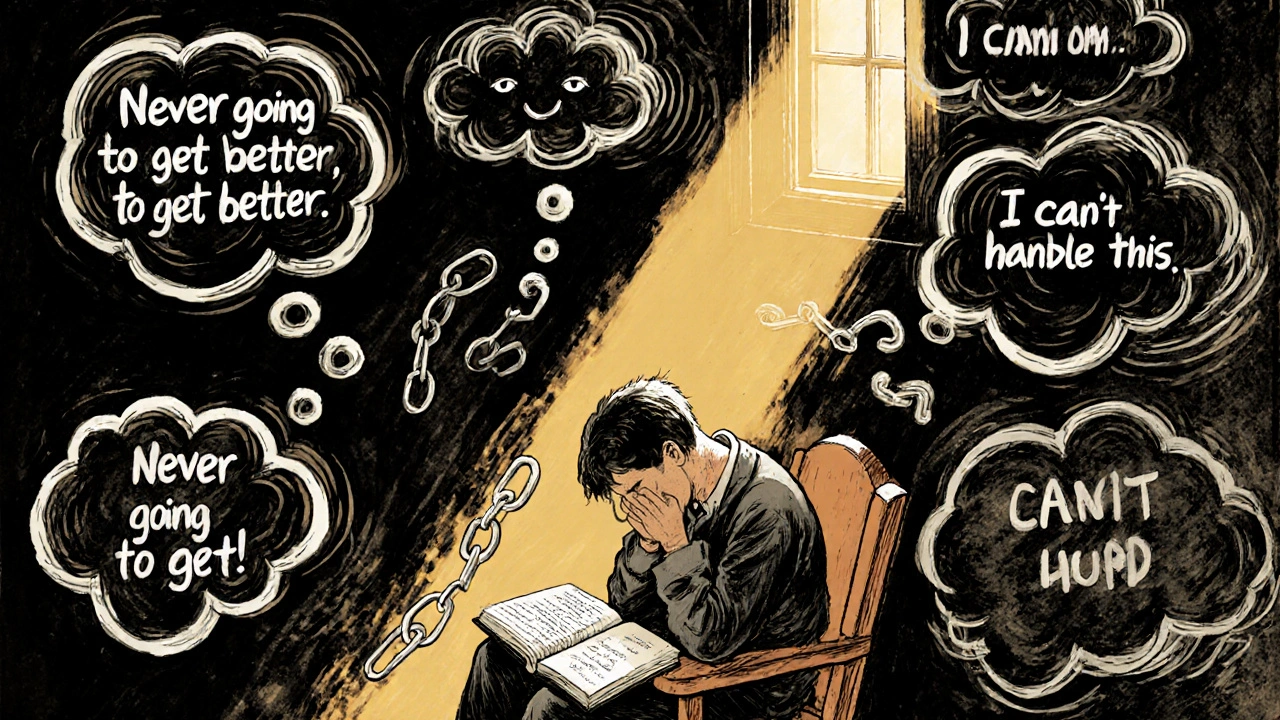
When your pain feels like it’s taking over your whole life - when every twinge makes you think, “This is never going to get better,” or “I can’t handle this anymore,” - you’re not just feeling physical discomfort. You’re caught in a mental trap called pain catastrophizing. It’s not weakness. It’s not exaggeration. It’s a real, measurable pattern of thought that makes pain feel worse, last longer, and steal more from your life than it should.
Research shows pain catastrophizing is one of the strongest predictors of poor outcomes in chronic pain. People who catastrophize are more likely to develop depression, avoid movement, take more medication, and miss work. But here’s the good news: this pattern isn’t permanent. Cognitive Behavioral Therapy, or CBT, has been proven to break it - and you don’t need to be a therapist to start using its tools.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing isn’t just being negative. It’s a specific trio of thoughts that lock into place when you’re in pain:
- Rumination: You can’t stop thinking about the pain. It loops in your head like a broken record: “Why won’t this stop? What if it gets worse? I can’t think about anything else.”
- Magnification: You blow the threat out of proportion. A small ache becomes “This is a sign something serious is happening.” A flare-up turns into “I’m going to end up in a wheelchair.”
- Helplessness: You feel powerless. “There’s nothing I can do. No one understands. I’m stuck.”
This isn’t just “thinking badly.” Brain scans show these thoughts actually light up areas linked to pain processing - meaning your mind is physically amplifying your pain. The Pain Catastrophizing Scale (PCS) is the standard tool used by clinicians to measure this. Scores above 30 out of 52 indicate clinically significant catastrophizing. If you’ve ever felt your pain controlling your emotions more than your body, you’re likely in that range.
How CBT Breaks the Cycle
CBT doesn’t try to make your pain disappear. It changes how you relate to it. Think of it like rewiring a faulty alarm system. The alarm (pain) is still there - but now you’re learning not to panic every time it goes off.
Studies from the Veterans Health Administration and Harvard Medical School show CBT reduces pain catastrophizing more effectively than any other psychological approach. In fact, when researchers looked only at people with high levels of catastrophizing, CBT was the only treatment that consistently delivered strong results. One 2023 study followed a 45-year-old woman with fibromyalgia. After 12 weeks of CBT, her PCS score dropped from 42 to 18. Her pain intensity fell by half. She went back to part-time work.
The magic isn’t in a pill or a machine. It’s in three simple, repeatable tools.
Tool 1: Self-Monitoring - Catching Thoughts Before They Spiral
The first step is awareness. You can’t change what you don’t notice.
Start a pain journal. Not just “pain level 7 today.” Instead, write down:
- What happened right before the pain spiked? (e.g., stood up from the chair, heard a loud noise, thought about tomorrow’s appointment)
- What thought popped into your head? (e.g., “I’m going to be like this forever,” “This means it’s getting worse,” “I can’t do anything right”)
- How did you feel emotionally? (anxious? hopeless? angry?)
- What did you do afterward? (avoided walking? called in sick? cried?)
Do this for 3-5 days. You’ll start seeing patterns. Maybe every time you think about work, your back pain spikes. Or every time your partner asks if you’re okay, you spiral into “I’m a burden.”
This isn’t about blaming yourself. It’s about seeing the connection between thought, feeling, and behavior. That’s the foundation of change.

Tool 2: Cognitive Restructuring - Rewriting the Script
Once you catch a catastrophic thought, challenge it. Not by telling yourself to “think positive.” That doesn’t work. Instead, ask:
- “What’s the evidence this thought is true?” (e.g., “I’ve had pain for 3 years - does that mean it’ll never change? Or has it improved on some days?”)
- “What’s a more balanced thought?” (e.g., “This is really hard right now, but it’s not the whole story. I’ve had better days before.”)
- “What would I say to a friend who had this thought?” (You’d probably be kinder to them than you are to yourself.)
Write down your new thought. Say it out loud. Post it on your mirror. Repeat it when the old thought shows up.
One veteran described it like this: “I used to think, ‘I’m broken.’ Now I say, ‘I’m healing, and it’s slow.’ That doesn’t fix my back, but it stops me from hating myself for having it.”
Tool 3: Behavioral Activation - Moving Despite the Fear
Pain catastrophizing doesn’t just live in your head - it shows up in your actions. You avoid activities because you fear they’ll make things worse. But avoidance makes pain stronger over time.
Behavioral activation means doing small, meaningful things even when you’re scared. Start tiny:
- Walk for 5 minutes instead of 20.
- Do one load of laundry instead of waiting until you “feel up to it.”
- Call a friend, even if you just say, “I’m having a rough day.”
Track it. Did your pain go up? Maybe. But did your mood improve? Did you feel a tiny bit more in control? That’s the win.
Studies show combining CBT with gentle movement - like walking or tai chi - gives the best results. You’re not trying to “fix” your pain. You’re rebuilding your life around it.

What If CBT Doesn’t Work Right Away?
It’s normal to feel frustrated. CBT isn’t a quick fix. Most people need 8-12 weeks to see real change. And some days - especially when pain is high - you won’t have the mental energy to use these tools.
That’s okay.
On those days, just do one thing: notice the thought without fighting it. Say to yourself, “Ah, there’s the ‘it’s never going to end’ story again.” Just naming it takes some of its power away.
Dropout rates are around 22% - often because people expect instant results. But if you stick with it, 78% of people on Reddit and in VA programs report significant relief in distress. You don’t need to be perfect. You just need to show up.
Who Benefits Most From CBT for Pain Catastrophizing?
CBT works best for people who:
- Have chronic pain that’s lasted more than 3 months
- Feel stuck in negative thought loops
- Want to reduce emotional suffering, not just physical pain
- Are willing to practice daily, even for 10 minutes
It’s less effective if you’re dealing with severe depression, untreated PTSD, or active substance use. In those cases, those issues need to be addressed first.
But if you’re tired of pain ruling your mind - and you’re ready to take back some control - CBT is your most proven path forward.
Where to Start Today
You don’t need a referral or a fancy clinic to begin.
- Download a free pain journal template (many VA websites offer them).
- Try the 5-minute “thought catch” exercise before bed.
- Look up “CBT for chronic pain” on the Veterans Health Administration’s Whole Health Library - it’s free, evidence-based, and designed for real people.
- Try apps like Curable or PainScale. They’ve helped over 450,000 people since 2020.
By 2025, 75% of pain clinics will screen for catastrophizing. That means the medical world is finally catching up to what patients have known for years: pain isn’t just in the body. It’s in the mind. And the mind can be trained.
You’re not broken. You’re caught in a pattern. And patterns can be changed - one thought, one small action, one day at a time.

Peter Lubem Ause
November 30, 2025 AT 15:59Just wanted to say this post is a game-changer. I’ve been living with chronic back pain for six years, and I didn’t realize how much my thoughts were making it worse. The three tools you laid out? Simple, but they actually work. I started journaling last week - not perfect, but I caught myself thinking ‘I’ll never walk without pain again’ and replaced it with ‘This is hard, but I’ve had good days before.’ It didn’t fix everything, but it gave me a breath. Thank you.
Joy Aniekwe
December 2, 2025 AT 09:31Oh wow. Another ‘CBT will save you’ post. Because clearly, if you’re just *thinking* about pain wrong, that’s why you’re disabled. Maybe if your pain wasn’t so severe, you’d have the energy to journal. But hey, at least your mind’s not broken - just your body.
gerardo beaudoin
December 4, 2025 AT 00:05lol i read this and thought ‘this is exactly what my PT told me’ - but she didn’t call it ‘catastrophizing’ so i thought i was just being dramatic. turns out i was. the thought-replacement thing? i started saying ‘this sucks right now’ instead of ‘i’m ruined’ and honestly? it helped more than the meds. no joke.
Mary Kate Powers
December 4, 2025 AT 09:51Thank you for writing this with so much care. I’ve been teaching pain management to seniors for years, and this is the clearest breakdown I’ve seen. The behavioral activation part? That’s the one people overlook. They think rest is healing - but movement, even tiny, is the real medicine. Keep sharing this.
Andrew Keh
December 5, 2025 AT 13:36It’s not about being positive. It’s about being honest. I used to think if I didn’t fight the pain, I was giving up. Turns out, I was just exhausting myself. Now I notice the thoughts. I don’t fight them. I just let them pass. Like clouds. And the pain? It’s still there. But it doesn’t own me anymore.
Sara Shumaker
December 6, 2025 AT 12:55I’ve been sitting with this for a while. The idea that pain isn’t just a signal - it’s a story we keep telling ourselves - it’s profound. We treat pain like a broken pipe, but what if it’s more like a song we’ve learned to play on repeat? CBT doesn’t mute the song. It teaches us to hum a different harmony. That’s revolutionary. Not because it’s new - but because we’re finally listening.
Richard Thomas
December 8, 2025 AT 02:26While the general sentiment is commendable, the empirical foundation of the cited 2023 fibromyalgia case study is insufficient for broad generalization. The sample size is n=1, and the PCS score reduction, while statistically notable, lacks longitudinal follow-up data. Furthermore, the assertion that ‘78% of people on Reddit’ report relief is methodologically unsound - Reddit is not a validated clinical population sample. One must be cautious in conflating anecdotal testimony with evidence-based medicine.
Steven Howell
December 8, 2025 AT 08:20As someone who worked with veterans at the VA for 15 years, I can confirm: CBT for pain catastrophizing is the single most underused tool in chronic pain care. We had patients who couldn’t get out of bed - after 10 weeks of daily journaling and one 5-minute walk, they started cooking again. Not because the pain vanished. Because they stopped letting it dictate their worth. This post? It’s the real deal.
tushar makwana
December 9, 2025 AT 07:23in india we dont really talk about pain like this... we just say ‘sab kuch kismat se hai’ but this made me think... maybe its not just fate... maybe my mind is playing tricks on me too. i tried writing one thought today... ‘this knee hurts’... then i wrote ‘but i still walked to the market’... small thing. but i felt less alone. thank you
LINDA PUSPITASARI
December 10, 2025 AT 13:51OMG I JUST DID THE JOURNAL THING AND I CRIED 😭 I didn’t realize I was saying ‘I’m a burden’ every time my husband asked if I needed help… and then I’d shut down… and he’d get sad… and then I’d feel worse… this isn’t just about pain - it’s about love too. I’m gonna try the ‘what would I say to a friend’ thing tomorrow. I’m so tired of being my own worst enemy
Scott Collard
December 11, 2025 AT 21:24You’re missing the point. The real issue is the medical system’s failure to validate pain. CBT doesn’t fix structural damage. It just teaches people to accept suffering as normal. That’s not healing. That’s resignation.