Kidney Function & Drug Dosing Calculator
Calculate Your Kidney Function
Results
Dosing Adjustment Guidance
When kidney function is reduced, your healthcare provider may need to adjust your medication dose. The exact adjustment depends on the specific drug and your overall health.
For many common medications, a 30-50% reduction in dose is needed when kidney function drops below 50 mL/min. This helps prevent side effects while maintaining therapeutic benefits.
Ever wonder why two people taking the same pill at the same dose have completely different experiences? One feels fine, the other ends up in the ER? It’s not luck. It’s not magic. It’s pharmacokinetics - the science of what your body does to a drug. This isn’t just for doctors and pharmacists. If you’re on medication, even once, this affects you.
What Happens When You Swallow a Pill?
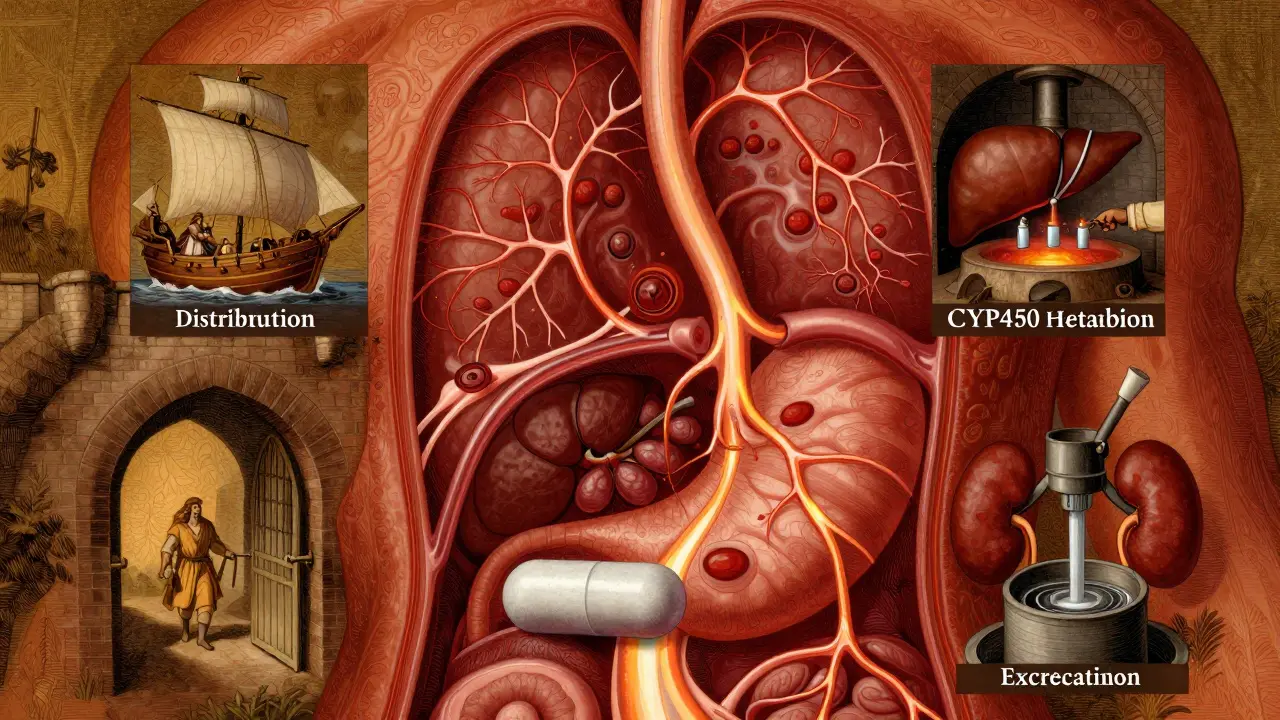
When you take a drug, whether it’s a pill, injection, or patch, your body doesn’t just accept it. It goes through four stages: Absorption, Distribution, Metabolism, and Excretion. Together, they’re called ADME. Think of it like a delivery system with checkpoints.
First, absorption. This is how the drug gets into your bloodstream. If you swallow a pill, it has to pass through your stomach and intestines. But not everything makes it. Your gut pH, how fast food moves through you, and even certain proteins like P-glycoprotein can block or slow absorption. For example, some antibiotics are absorbed 30-70% less if taken with calcium-rich foods. That’s why your doctor tells you to take certain meds on an empty stomach.
Not all drugs are swallowed. An IV shot? That’s 100% absorption - straight into your blood. A patch? Slow and steady. A nasal spray? Faster than a pill. The route changes everything.
Where Does the Drug Go?
Once in your blood, the drug gets distributed. This isn’t random. Some drugs stick to proteins in your plasma. Warfarin, for example, is 98% bound to albumin. That means only 2% is free to work. If another drug kicks off that bound warfarin, suddenly you’ve got too much active drug in your system. That’s how bleeding risks spike.
Other drugs slip into tissues - fat, muscle, even your brain. That’s measured by volume of distribution (Vd). A low Vd means the drug stays mostly in your blood. A high Vd? It’s soaking into your organs. That’s why some drugs affect your liver more than your heart, and why others make you drowsy even if they’re supposed to treat your joints.
Your Liver: The Drug’s Worst Enemy
Metabolism happens mostly in your liver. Enzymes - especially the CYP450 family - break down drugs so your kidneys can flush them out. CYP3A4 alone handles about half of all prescription meds. But here’s the catch: your genes decide how fast this enzyme works.
Some people are slow metabolizers. For example, 3-10% of Caucasians have a CYP2D6 variant that can’t turn codeine into morphine. They get no pain relief. Others are ultra-rapid - they turn codeine into morphine too fast. That’s how some people overdose on standard doses.
Drugs can also interfere with each other. Take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug). Clarithromycin blocks CYP3A4. Simvastatin builds up. Risk of muscle damage? Goes from 0.04% to 0.5%. That’s a 12-fold increase. And most people don’t know they’re taking this combo.
How Your Body Gets Rid of It
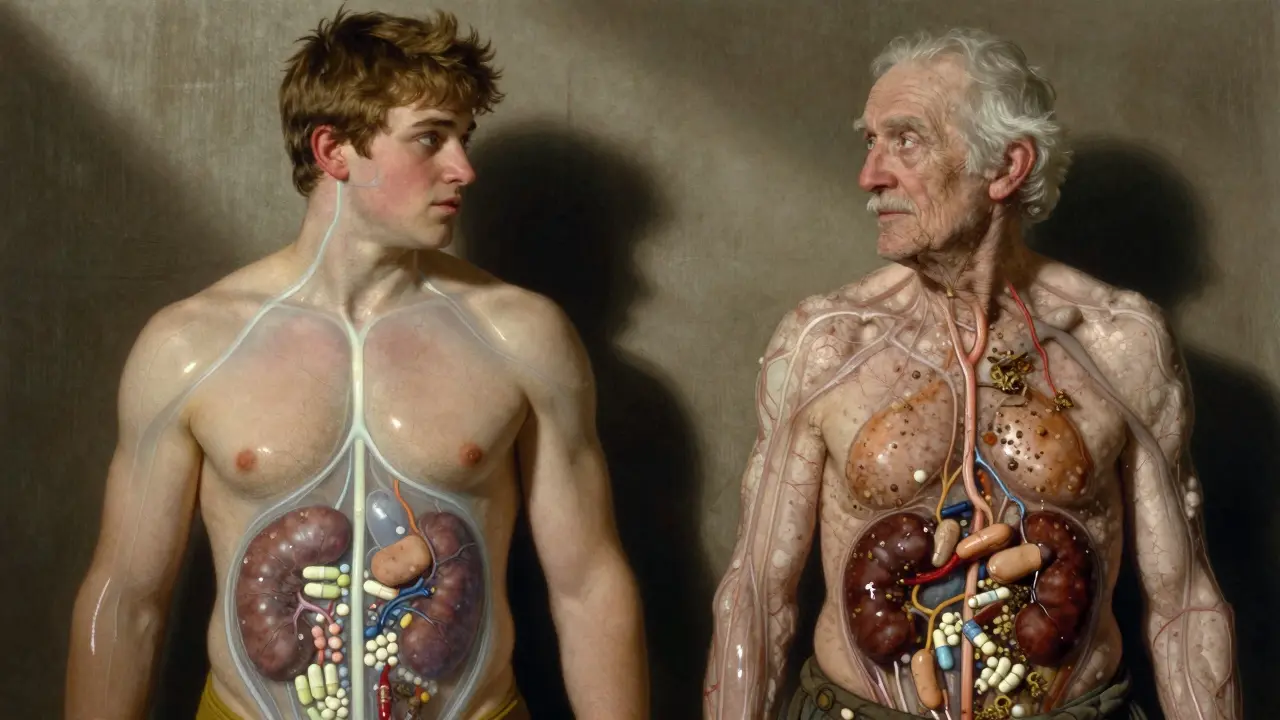
Excretion is mostly through the kidneys. Your kidneys filter blood. If your kidney function drops - say, from age, diabetes, or dehydration - drugs don’t clear as fast. That’s why older adults get side effects more often. Their kidneys clear drugs 30-40% slower than younger people.
Normal kidney filter rate? 90-120 mL/min. In end-stage kidney disease? It can drop below 15 mL/min. That’s why vancomycin (an antibiotic) can cause kidney damage if dosed like it’s for a 30-year-old. A 78-year-old with a creatinine clearance of 25 mL/min? They need a much lower dose. But many hospitals still use standard charts. That’s how patients end up with rising creatinine levels and hospital stays.
Side Effects Aren’t Random - They’re Predictable
Side effects happen when drug levels go too high. Too low? No effect. Too high? Toxicity.
Phenytoin (an epilepsy drug) has a narrow window. At 10-20 mcg/mL? Works. Above 20 mcg/mL? 30% of patients get tremors, dizziness, even coma. At therapeutic levels? Only 2% have side effects. That’s why doctors check blood levels.
And it’s not always the original drug. Diazepam (Valium) breaks down into desmethyldiazepam - a metabolite with a 100-hour half-life. In young people? Fine. In elderly? It builds up. That’s why older adults fall more often on benzodiazepines. It’s not the drug. It’s the leftover stuff.
Warfarin? Another classic. A single gene variant in CYP2C9 can make you 5 times more likely to bleed on a standard dose. That’s why some clinics now test for it before prescribing. It’s not optional anymore - it’s standard practice for high-risk drugs.
Why Age, Weight, and Other Drugs Matter So Much
Here’s the truth: there’s no such thing as a standard dose. There’s only a starting point.
People over 65 have 30-50% less liver function. Their kidneys work slower. They’re often on 5+ meds. That’s why 1 in 3 adverse drug reactions happen in older adults. And it’s not because they’re “noncompliant.” It’s because the dose was never adjusted.
Obesity? Fat changes how drugs distribute. A 120kg person doesn’t need 2x the dose of a 60kg person - but they often get it. That’s because dosing is based on weight, but not on body composition. Muscle vs. fat changes drug behavior.
And what you eat? Grapefruit juice? It blocks CYP3A4. Same as clarithromycin. One glass can turn a safe statin dose into a dangerous one. It’s not a myth. It’s science.
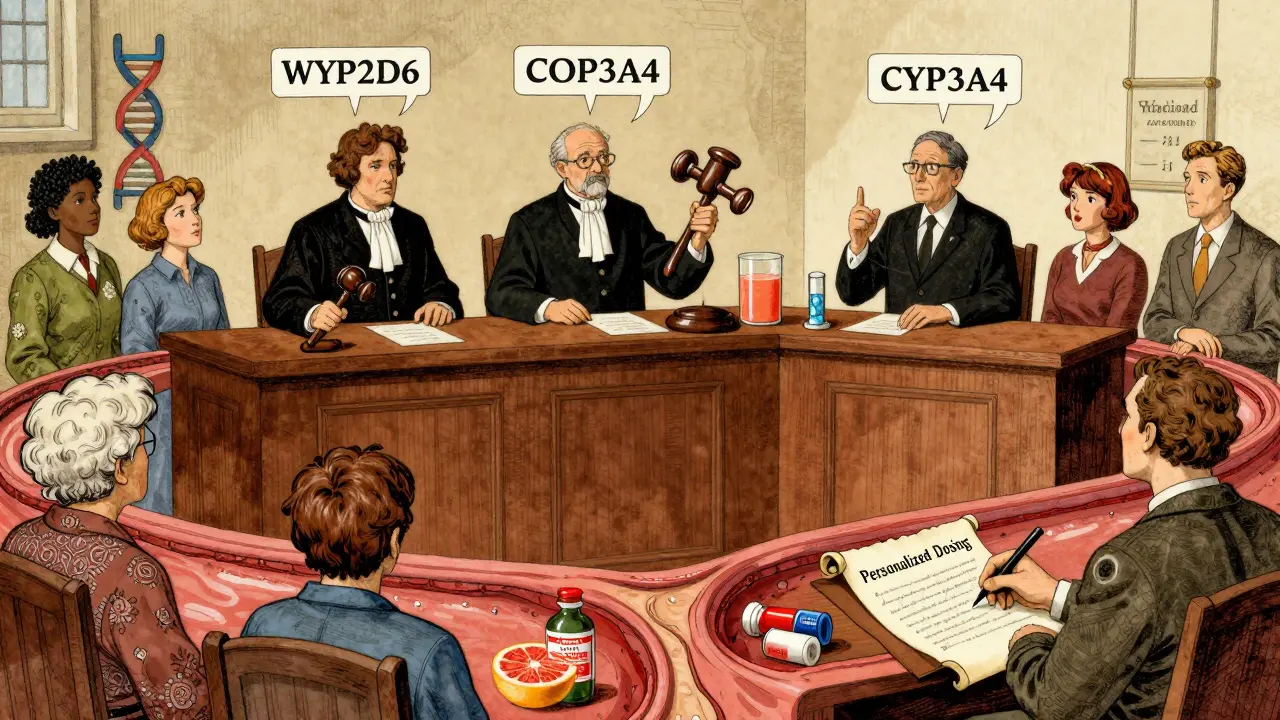
What’s Changing Now? Personalized Dosing
Pharmacokinetics is no longer guesswork. It’s data-driven.
AI tools like DoseMeRx are now FDA-approved. They take your age, weight, kidney function, genetics, and current meds - then spit out a custom dose. For vancomycin, they cut dosing errors by 62%. That’s huge.
Regulators are catching up. The FDA now requires PBPK modeling (computer simulations of how drugs behave in virtual populations) for nearly all new cancer drugs. The EMA launched PK4All to build global databases for rare diseases. And the NIH is spending $185 million to fix the biggest gap: most pharmacokinetic studies still use young, white, male volunteers - even though 85% of patients aren’t.
Even your gut bacteria matter now. Researchers found 15-20% of oral drugs are changed by gut microbes before they even reach your liver. That’s why two people on the same drug can have totally different outcomes - one has a healthy microbiome, the other doesn’t.
What You Can Do
You don’t need to be a scientist to use this info.
- Know your meds. If you’re on warfarin, ask if your dose was adjusted for your age or kidney function.
- Tell your doctor about all supplements. St. John’s Wort? It speeds up metabolism. It can make birth control, antidepressants, or transplant drugs fail.
- Don’t ignore side effects. If you feel dizzy after a new drug, don’t just wait it out. Ask: “Could this be a pharmacokinetic issue?”
- Ask about testing. For drugs like clopidogrel, abacavir, or codeine, genetic testing is available and prevents serious reactions.
Medication isn’t one-size-fits-all. Your body isn’t a textbook. It’s unique. Understanding how it handles drugs isn’t just academic - it’s life-saving.
What does pharmacokinetics mean?
Pharmacokinetics is the study of how your body absorbs, distributes, metabolizes, and excretes a drug. It answers questions like: How much of the drug reaches your bloodstream? How long does it last? Where does it go? And how fast is it removed? This is different from pharmacodynamics, which looks at how the drug affects your body.
Why do some people have worse side effects than others?
Because everyone’s body processes drugs differently. Genetics affect how fast your liver breaks down meds. Kidney function changes with age. Other drugs can block or speed up metabolism. Even your diet and gut bacteria play a role. A dose that’s safe for one person can be toxic for another.
Can I test my body’s ability to process drugs?
Yes, in some cases. Genetic tests can identify variants in enzymes like CYP2D6 or CYP2C9 that affect how you metabolize common drugs like codeine, warfarin, or clopidogrel. Therapeutic drug monitoring (TDM) measures actual drug levels in your blood - often used for epilepsy meds, antibiotics, and antidepressants. These aren’t routine for everyone, but they’re standard for high-risk medications.
Does taking meds with food really matter?
Yes. Food can block absorption (like calcium with antibiotics) or boost it (like fatty meals with some HIV meds). Grapefruit juice blocks liver enzymes and can raise drug levels dangerously. Always check the label or ask your pharmacist. The timing and type of food can change how well your drug works - or how dangerous it becomes.
Why are older adults more at risk for drug side effects?
As we age, liver metabolism drops by 30-50%, and kidney clearance falls by 30-40%. Fat increases and muscle decreases, changing how drugs are distributed. Older adults also take more medications - increasing the chance of dangerous interactions. What was a safe dose at 40 might be toxic at 75. Doses should be lowered, not just repeated.
Is pharmacokinetics only for serious drugs?
No. Even common drugs like ibuprofen, acetaminophen, or antihistamines can build up if your kidneys are slow. A 70-year-old on daily ibuprofen for arthritis might not realize their kidney function has dropped. That’s how liver damage or stomach bleeding happens. Pharmacokinetics matters for every medication - not just the ones on black-box warnings.
Final Thought
Your body isn’t a machine with a fixed setting. It’s a living system. And drugs? They’re chemicals that interact with it - sometimes beautifully, sometimes dangerously. The better you understand how your body handles them, the safer you are. Ask questions. Demand better. Your life depends on it.