Key Takeaways
- Porphyria is a group of genetic disorders that disrupt heme production, often striking the nervous system.
- Acute attacks cause nerve pain, seizures, and mental changes; triggers include drugs, fasting, and hormonal shifts.
- Diagnosis relies on urine, blood and stool porphyrin tests; early detection prevents lasting nerve damage.
- Treatment combines hemin infusion, safe drug choices, and lifestyle tweaks to keep attacks at bay.
- Regular monitoring of liver function and neurological status is essential for long‑term health.
What is Porphyria?
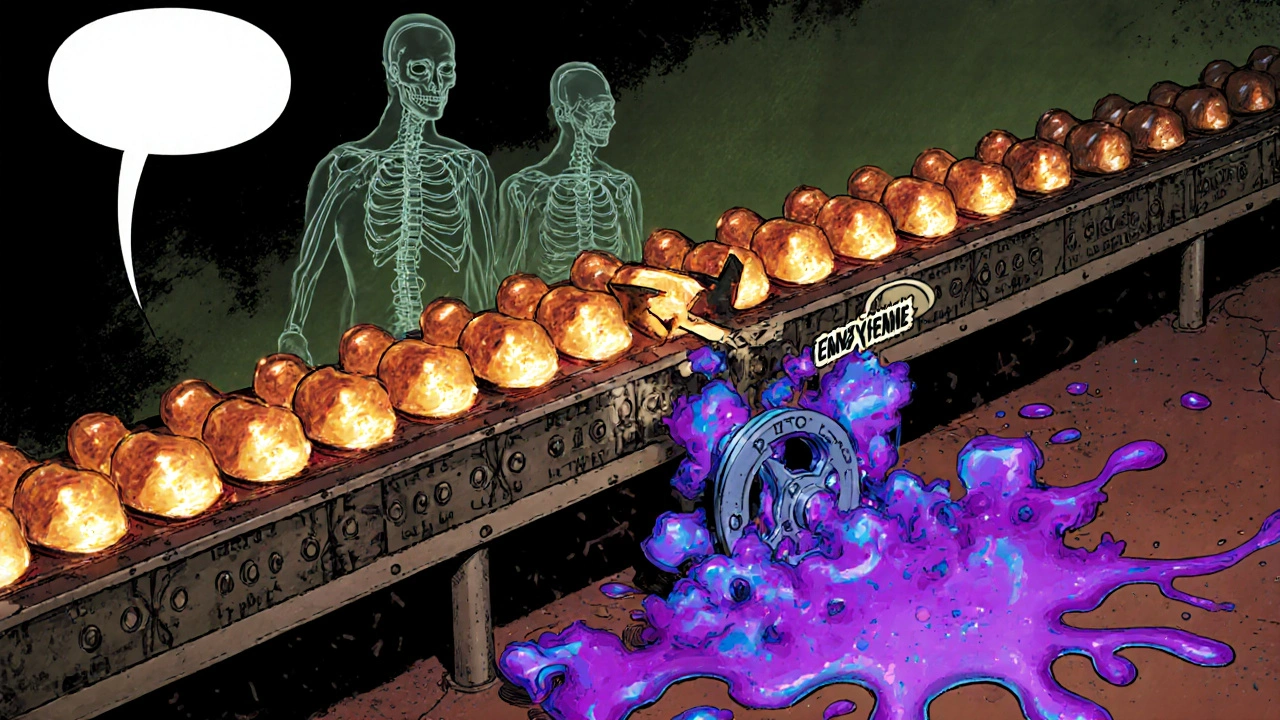
When you hear porphyria, think of a broken assembly line for heme, the iron‑rich molecule that lets blood carry oxygen. Porphyria is a family of inherited or acquired disorders that impair the enzymes responsible for heme biosynthesis. The blockage forces intermediate chemicals-porphyrins and their precursors-to pile up in the liver, skin, and nervous tissue, producing a wide‑ranging set of symptoms.
How Heme Biosynthesis Works and Where It Breaks
The heme pathway starts in the mitochondria of liver cells and runs through eight steps. Each step needs a specific enzyme; miss one, and the whole line stalls. Heme biosynthesis is the multi‑step chemical process that creates heme, a component of hemoglobin, cytochromes, and several enzymes. When an enzyme such as porphobilinogen deaminase (defective in acute intermittent porphyria) or uroporphyrinogen decarboxylase (defective in porphyria cutanea tarda) falters, toxic precursors overflow into the bloodstream.
Types of Porphyria with Neurological Impact
| Porphyria | Primary organ affected | Typical triggers | Neurological involvement |
|---|---|---|---|
| Acute Intermittent Porphyria (AIP) | Liver | Hormonal changes, fasting, barbiturates, sulfonamides | Severe, includes peripheral neuropathy, seizures, confusion |
| Hereditary Coproporphyria (HCP) | Liver | Alcohol, smoking, certain antibiotics | Similar to AIP but milder; can cause motor weakness |
| Variegate Porphyria (VP) | Liver & skin | Stress, infections, certain drugs | Peripheral neuropathy and acute attacks comparable to AIP |
| Porphyria Cutanea Tarda (PCT) | Skin | Iron overload, hepatitis C, estrogen therapy | Usually no acute neurological symptoms; chronic photosensitivity dominates |
How Porphyria Affects the Nervous System
Neurological damage in porphyria stems from three linked mechanisms:
- Neurotoxic porphyrin precursors-Compounds like ALA (δ‑aminolevulinic acid) cross the blood‑brain barrier and irritate neurons, leading to pain and altered mental status.
- Energy failure-Heme is essential for cytochromes in mitochondria; a shortage stalls ATP production, making long nerves especially vulnerable.
- Inflammatory cascade-Accumulated porphyrins trigger oxidative stress, which amplifies nerve inflammation and can cause demyelination.
These processes explain why patients report a “band‑like” abdominal pain that precedes tingling in the hands, foot drop, or even seizures.
Recognizing Neurological Symptoms Early
Spotting the nerve‑related warning signs can prevent irreversible damage. Common clues include:
- Sudden, severe abdominal or back pain without an obvious cause.
- Tingling, numbness, or “pins‑and‑needles” sensations starting in the fingers or toes.
- Muscle weakness that progresses upward, sometimes resulting in difficulty walking.
- Speech slurring, confusion, or hallucinations during an attack.
- Seizures-often preceded by visual disturbances or a throbbing headache.
If any of these appear after starting a new medication, a low‑carb diet, or hormonal therapy, seek a porphyria work‑up right away.
Diagnosis and Monitoring
Laboratory testing remains the gold standard. The first step is a spot urine sample collected at the height of symptoms. Elevated levels of porphobilinogen (PBG) and ALA confirm an acute attack. Urine porphobilinogen is a diagnostic marker that spikes dramatically during an acute porphyria episode. Follow‑up tests include:
- Quantitative porphyrin analysis in stool (helps differentiate AIP from HCP or VP).
- Serum ferritin and iron studies (especially important for PCT).
- Genetic testing for mutations in the HMBS gene (AIP) or CPOX gene (HCP) to confirm hereditary forms.
- Electrodiagnostic studies (EMG, nerve conduction) if neuropathy persists after the acute phase.
Regular monitoring of liver enzymes, renal function, and psychiatric status is advised because chronic porphyrin accumulation can affect these systems over time.

Managing Neurological Complications
Therapy focuses on two fronts: stopping the acute surge and protecting nerves.
- Hemin infusion-A synthetic form of heme that restores feedback inhibition, rapidly lowering ALA and PBG levels. Typically given 3-4mg/kg daily for 4-5 days during an attack.
- Avoiding triggers-Maintain a balanced diet (avoid prolonged fasting), limit alcohol, and use only “porphyria‑safe” medications (lists are available from specialist registries).
- Symptomatic control-Analgesics that don’t interfere with the cytochrome P450 system (e.g., acetaminophen), anti‑seizure drugs like gabapentin, and short‑acting benzodiazepines for anxiety.
- Physical therapy-Early rehab helps recover strength after neuropathy; gentle resistance exercises prevent muscle wasting.
- Long‑term prophylaxis-Some patients benefit from weekly sub‑cutaneous hemin or low‑dose glucose infusions to keep the pathway humming.
Because the nervous system’s recovery can be slow, regular follow‑up with a neurologist and a metabolic specialist ensures any lingering deficits are addressed promptly.
Living with Porphyria: Practical Tips
Daily habits can make a huge difference:
- Carry a “porphyria emergency card” listing safe medications and contact details.
- Stay hydrated and avoid drastic diets; a snack rich in complex carbs can blunt an attack.
- Schedule routine blood work every 6‑12 months to track liver health.
- Inform your dentist and surgeon about your condition before any procedure.
- Join support groups-sharing experiences often uncovers hidden triggers.
Frequently Asked Questions
Can porphyria cause permanent nerve damage?
If an acute attack is treated promptly, most nerve symptoms improve within weeks to months. However, severe or repeated attacks can lead to lasting neuropathy, especially in the lower limbs.
Which medications are safest for people with acute porphyria?
Analgesics such as acetaminophen, anti‑emetics like ondansetron, and certain antihistamines are considered low‑risk. Always check the latest porphyria‑safe drug list before starting new meds.
Is there a genetic test for porphyria?
Yes. Testing for mutations in the HMBS gene confirms acute intermittent porphyria, while CPOX, PPOX, and UROD gene panels cover other hereditary forms.
Do lifestyle changes really help prevent attacks?
Absolutely. Maintaining steady carbohydrate intake, avoiding alcohol, and steering clear of known drug triggers reduce the frequency of acute episodes by up to 60% in many patients.
What is the role of the liver in porphyria?
The liver houses most of the heme‑producing enzymes. Enzyme defects there cause a buildup of toxic precursors that spill into the bloodstream and reach the nervous system.

Roberta Makaravage
October 16, 2025 AT 20:45Understanding porphyria isn’t just about biochemistry; it’s a moral imperative to recognize how hidden metabolic failures can devastate lives 😔. The cascade of neurotoxic precursors that breach the blood‑brain barrier illustrates a failure of our medical systems to prioritize rare diseases. When you consider that a simple carbohydrate snack can blunt an attack, the ethical responsibility of clinicians becomes crystal clear. Moreover, the fact that many patients suffer for years before a correct diagnosis shines a light on systemic neglect. Ethical healthcare must integrate proactive screening for at‑risk individuals, especially those with familial histories. It’s not enough to treat the attack; we must dismantle the barriers that delay diagnosis. In my view, the only justified response is a universal, subsidized porphyria panel for anyone presenting with unexplained abdominal pain. This would reduce the needless suffering and align medical practice with the principle of beneficence. 🌟
James Falcone
October 28, 2025 AT 09:43Honestly, the U.S. health system could learn a thing or two from other countries about handling rare disorders like porphyria. We have the tech and the labs, yet patients still wait months for a proper work‑up. It’s a shame that bureaucracy drags on while nerves deteriorate. Cutting red tape and giving doctors clear guidelines on safe meds would save money and pain. Our troops and workers deserve better access to these life‑saving hemin infusions without jumping through hoops. Let’s make it happen.
Frank Diaz
November 8, 2025 AT 23:46The brain, as a vessel for consciousness, mirrors the delicate balance of heme synthesis. When that balance is tipped, the resulting neurotoxicity reveals our fragile grasp on self‑control. Porphyria attacks expose how quickly the body can betray its own purpose, a lesson in humility. The seizures and confusion are not mere symptoms but existential warnings. They remind us that every metabolic pathway is a thread in the tapestry of identity. Ignoring these signals is equivalent to denying our own mortality. Thus, we must respect the biochemical truth before us, not merely treat it as a inconvenience.
Mary Davies
November 20, 2025 AT 13:50The description of tingling fingers and sudden abdominal pain reads like a dramatic scene from a medical thriller. Yet for patients, it’s a daily nightmare that can strike without warning. The way the article lays out the triggers makes it clear that lifestyle choices hold real power. It’s both terrifying and empowering to realize a simple carb snack can halt an attack. I admire the thoroughness of the recommendations, especially the emphasis on safe medication lists. It gives hope that with vigilance, the worst can be avoided.
Valerie Vanderghote
December 2, 2025 AT 03:53Let me just say that the whole discussion about porphyria and the nervous system is far more intricate than most people give it credit for, and I’m going to unpack every layer because we deserve a full picture. First, the biochemical pathway is a cascade of eight enzymatic steps, each a potential point of failure, and when one falters, you get a buildup of highly reactive intermediates that do more than just sit around-they actively irritate neuronal membranes, leading to that classic “pins‑and‑needles” sensation that patients describe. Second, the fact that these intermediates, especially δ‑aminolevulinic acid, can cross the blood‑brain barrier means the central nervous system is directly assaulted, which explains why seizures and mental status changes are such hallmark features. Third, the energy failure caused by insufficient heme in mitochondrial cytochromes isn’t a trivial footnote; it translates into reduced ATP production, and nerves, being long and metabolically demanding, are among the first to suffer, leading to peripheral neuropathy that can become irreversible if attacks are recurrent. Fourth, the inflammatory cascade-oxidative stress, cytokine release, demyelination-adds another layer, turning a metabolic glitch into an outright neuroinflammatory process. Fifth, the triggers aren’t obscure; they’re common in modern life-fasting, hormonal shifts, certain antibiotics, even some over‑the‑counter pain relievers-so awareness is crucial. Sixth, the diagnostic work‑up isn’t just a single urine test; it’s a coordinated effort involving spot urine PBG, stool porphyrin analysis, serum ferritin, and often genetic panels to pinpoint the exact variant, which then guides long‑term management. Seventh, while hemin infusion is the gold standard for acute attacks, it’s not a panacea; the infusion must be timed correctly, dosed properly (3‑4 mg/kg), and paired with supportive measures like glucose loading to suppress the pathway’s upstream enzymes. Eighth, lifestyle modifications-steady carbohydrate intake, avoiding alcohol and known drug triggers-are not just advice but proven strategies that can reduce attack frequency by up to 60 %. Ninth, the importance of multidisciplinary follow‑up can’t be overstated; neurologists, hepatologists, and metabolic specialists must coordinate to monitor liver function, renal health, and neuro‑rehabilitation. Tenth, the psychosocial impact-patient anxiety, potential for depression, and the need for support groups-must be addressed because the disease doesn’t live in a vacuum. Eleventh, the practical tip of carrying an emergency card is a simple yet life‑saving action. Twelfth, informing every surgeon or dentist beforehand prevents iatrogenic triggers that could precipitate a crisis. Thirteenth, let’s not forget that while many patients recover fully after an acute episode, repeated assaults can lead to permanent neuropathy, especially in the lower limbs, underscoring the urgency of early intervention. Finally, all of this underscores a singular truth: porphyria is not just a hematologic curiosity; it’s a systemic disorder that demands a comprehensive, proactive, and patient‑centered approach. If anyone still thinks this is a niche issue, they need to read the literature more closely.
Michael Dalrymple
December 13, 2025 AT 17:56From a coaching perspective, the best approach to managing porphyria‑related neuropathy is to combine medical treatment with structured rehabilitation. Begin with gentle range‑of‑motion exercises as soon as the acute attack subsides to preserve joint flexibility. Progress to low‑impact strength training, focusing on the distal muscles that are often first affected. Incorporate balance drills to prevent falls, especially if foot drop is present. Throughout, monitor the patient’s energy levels to avoid overexertion, which could trigger another metabolic surge. Regular reassessment ensures the program adapts to the evolving neurological status. This balanced regimen, paired with timely hemin infusions, offers the greatest chance for functional recovery.
Carissa Padilha
December 25, 2025 AT 08:00What they don’t tell you is that the pharmaceutical industry has a vested interest in keeping porphyria under the radar. The cheap glucose infusions are pushed as a miracle cure, but the real profit lies in patented hemin products sold at astronomical prices. Meanwhile, clinical trials are subtly steered to highlight side effects of the very drugs that trigger attacks, creating a feedback loop of dependence. It’s no coincidence that the most vulnerable patients are the ones most likely to be swayed by aggressive marketing. Question everything, especially when lifesaving treatments are involved.
Richard O'Callaghan
January 5, 2026 AT 22:03i think its crazzzy how many poephyria cases go unrecoginzed. the simsple labs like urine test ar cheap, but hospitals keep waitng for months. ppl get nerve damge bc of this. its realy sad.
Nickolas Mark Ewald
January 17, 2026 AT 12:06Good overview, very helpful.
Chris Beck
January 29, 2026 AT 02:10Porphyria is a problem. It is serious. The nervous system is affected; treatment is needed. Patients should see doctors, get tests, avoid triggers, and use hemin if needed.