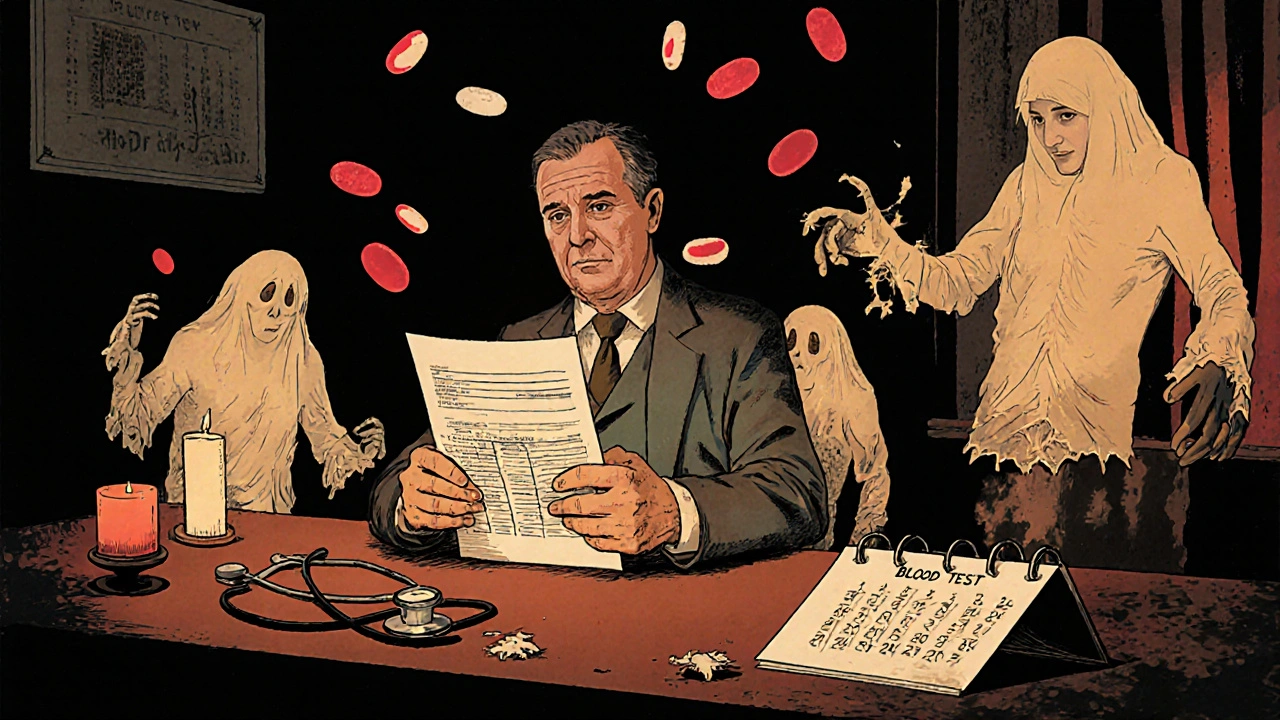
When you get a blood count, a standard lab test that measures the number and types of cells in your blood. Also known as complete blood count, it’s one of the most common tests doctors order because it shows if something’s off—before you even feel sick. This test doesn’t just count cells; it tells a story about your immune system, oxygen transport, and even hidden inflammation.
Most people know their hemoglobin, the protein in red blood cells that carries oxygen levels, but few realize how much drugs like statins, antibiotics, or chemotherapy can shift those numbers. For example, some antibiotics can drop your white blood cell count, making you more vulnerable to infections. Others, like allopurinol, a medication used to lower uric acid in gout and kidney disease, can trigger rare but serious drops in blood cell production. Even something as simple as long-term NSAID use can quietly affect your platelets or cause minor bleeding that shows up in your red cell count.
Your white blood cells, the body’s frontline defenders against infection tell you if your immune system is fighting something—maybe a virus, an autoimmune flare, or even a hidden cancer. A high count might mean you’re sick right now. A low count could mean your body’s running on empty, especially if you’re on meds that suppress bone marrow. And if you’re managing chronic kidney disease, a condition where kidneys can’t filter waste or make enough red blood cells, your blood count becomes a daily monitor—not just a one-time check.
What you’ll find in these posts isn’t just theory. It’s real-world connections: how blood count changes with medications like Sinemet, Lincocin, or Abacavir; how kidney disease and gout treatments quietly reshape your cell levels; and why some people on long-term drugs need regular blood tests more than others. No fluff. Just what your numbers mean, why they matter, and what to ask your doctor next time you get your results.