When you hear hydroxyurea, a prescription medication used to treat sickle cell disease and certain blood cancers by reducing the production of abnormal blood cells. Also known as hydroxycarbamide, it's one of the few drugs proven to reduce painful crises in sickle cell patients and lower the risk of stroke in children. Unlike newer biologics, hydroxyurea has been around for decades—but it still works, and millions rely on it daily.
It’s not just for sickle cell. myeloproliferative disorders, a group of blood cancers where the bone marrow makes too many blood cells, including polycythemia vera and essential thrombocythemia also respond to hydroxyurea. Doctors use it to bring down high red blood cell or platelet counts, reducing the chance of clots, heart attacks, or strokes. It’s often the first choice because it’s oral, affordable, and well-studied. But it’s not magic—it takes weeks to show effects, and blood counts must be monitored closely. Side effects like low white blood cells or nausea are common, but manageable for most.
People often ask: are there better options? For sickle cell, crizanlizumab, a newer IV drug that prevents blood cells from sticking together and causing pain crises is an option, but it costs far more and requires monthly infusions. For some, voxelotor, a drug that helps red blood cells carry oxygen better works alongside hydroxyurea. In myeloproliferative disorders, ruxolitinib is used when hydroxyurea fails—but it’s expensive and can cause anemia. Hydroxyurea still holds ground because it’s effective, accessible, and doesn’t need special storage or equipment.
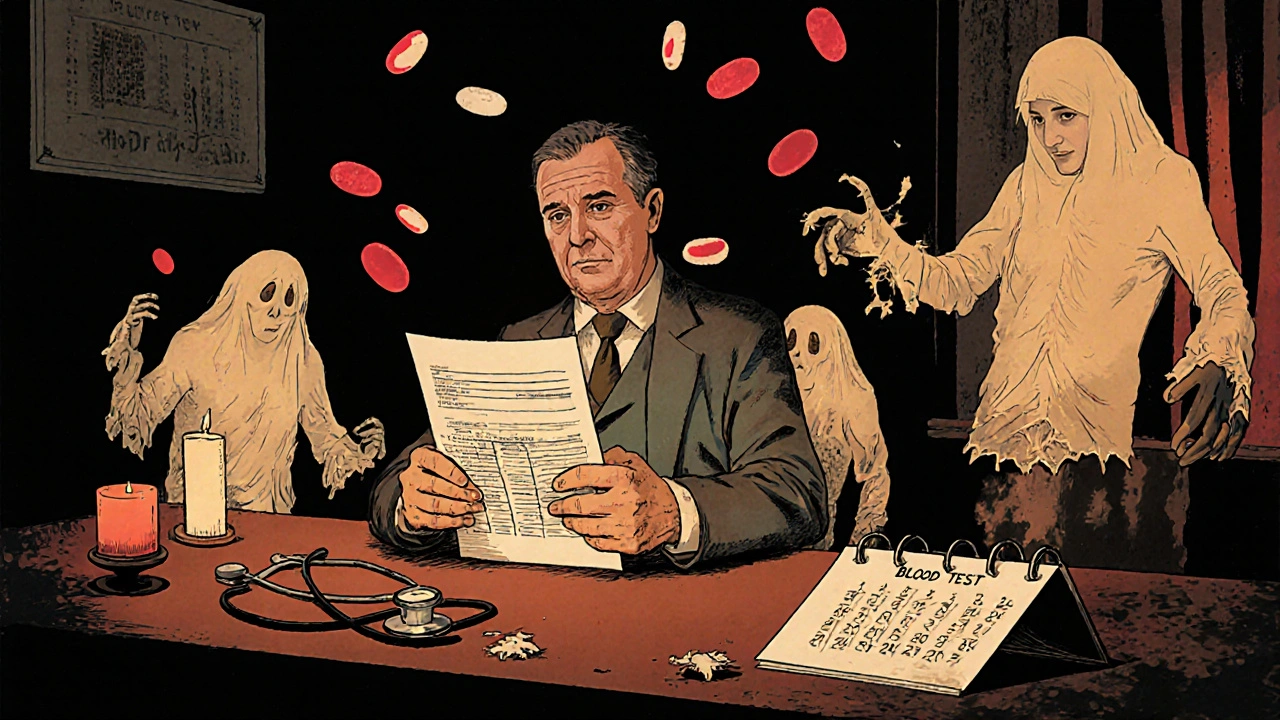
What you won’t find in most doctor’s offices is a full picture of how hydroxyurea fits into real-life care. Some patients use it for years without issues. Others switch because of side effects or fear of long-term risks. And while it’s not a cure, it changes lives—many kids with sickle cell who take it regularly can go to school without hospital visits. The posts below dig into exactly that: how hydroxyurea compares with other treatments, what real patients experience, how labs track its impact, and why some doctors hesitate to prescribe it. You’ll also find stories on managing side effects, what to do if it stops working, and how insurance handles it. This isn’t just a drug guide—it’s a practical map for anyone living with or caring for someone on hydroxyurea.