When you're taking hydroxyurea, a prescription medication used to treat sickle cell disease and certain types of leukemia by reducing the production of abnormal blood cells. Also known as Hydrea, it works by slowing down bone marrow activity—but that’s exactly why you need careful hydroxyurea monitoring. This isn’t a drug you start and forget. Without regular checks, it can drop your white blood cell count too low, leaving you vulnerable to infections, or reduce your platelets so much that you bruise easily or bleed without cause.
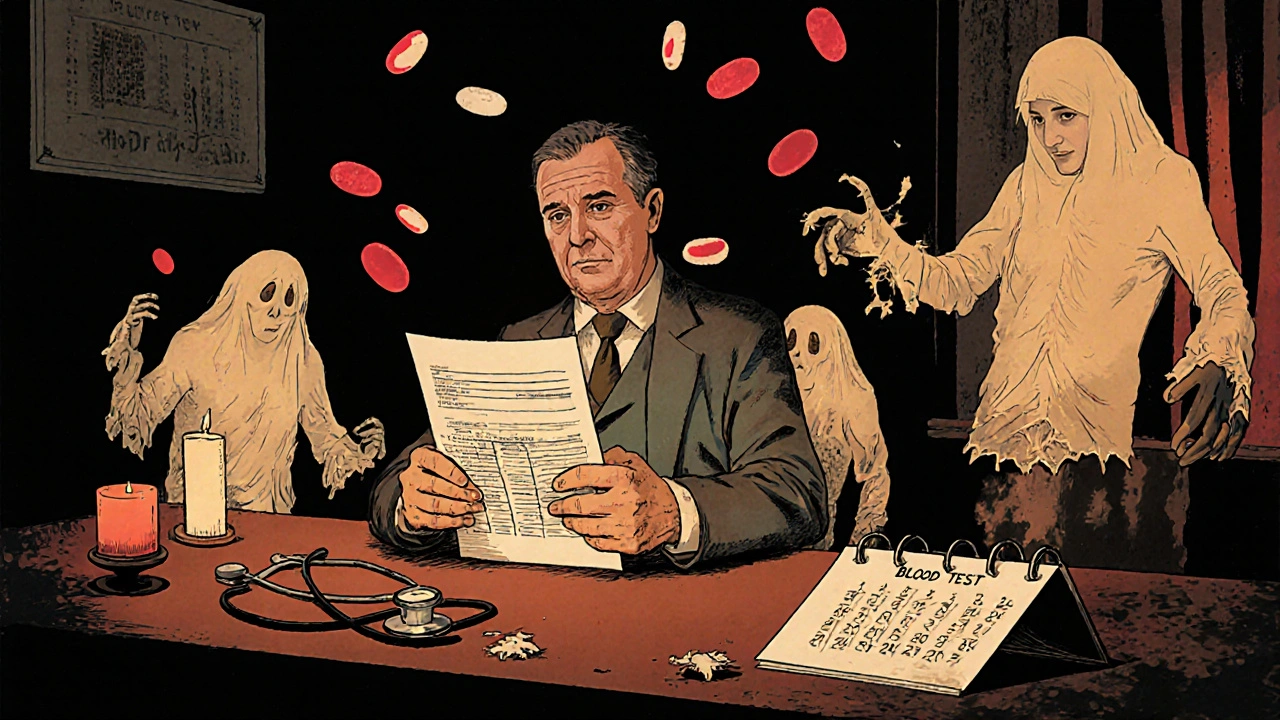
Doctors rely on three key blood tests to keep hydroxyurea safe: complete blood count (CBC), a routine lab test that measures red blood cells, white blood cells, and platelets, liver function tests, to catch early signs of liver stress from long-term use, and sometimes kidney function markers, since hydroxyurea is cleared through the kidneys and poor function can lead to drug buildup. Most patients get a CBC every 2 to 4 weeks when starting, then every 1 to 3 months once stable. If your white count falls below 4,000 or platelets drop under 100,000, your dose gets lowered—or paused. Skipping these tests is like driving with no speedometer.
Hydroxyurea monitoring isn’t just about avoiding danger—it’s about making sure the drug actually works. In sickle cell disease, the goal isn’t just to feel better, but to raise fetal hemoglobin levels enough to reduce painful crises. That takes time, and it takes tracking. Some people see results in 3 months; others need 6 or more. If your labs stay stable but you’re still having frequent pain episodes, your doctor might look at other factors: hydration, iron levels, or even whether you’re taking the drug exactly as prescribed. It’s not always the medication—it’s how it’s used.
You’ll also hear about skin changes, mouth sores, or nail darkening as side effects. These aren’t emergencies, but they’re signals. If your nails turn black or your skin gets unusually dark, tell your provider. These can be harmless, but they’re also signs your body is reacting to the drug. And if you develop a fever, sore throat, or unexplained bruising? Don’t wait. Call your doctor immediately. Those could mean your white blood cells have crashed.
What you find in the posts below isn’t just a list of articles—it’s a practical toolkit. You’ll see how hydroxyurea compares to newer treatments like voxelotor and crizanlizumab, how insurance often blocks access to regular lab tests, and what to do if your doctor won’t order the right blood work. There’s also real talk about managing side effects at home, how to talk to your pharmacist about dosage timing, and why some patients stop taking hydroxyurea not because it doesn’t work—but because no one ever taught them how to monitor it right.