Ever taken a pill and wondered if it really worked because you ate right after? You’re not alone. Millions of people take medications daily, but many don’t realize that what’s on their plate can make the difference between a drug working as it should - or doing nothing at all. Food doesn’t just fill your stomach. It changes how your body handles medicine. Some drugs work better with food. Others become useless or even dangerous if taken near a meal. The timing isn’t just a suggestion. It’s science.
Why Food Changes How Medicines Work
Your digestive system doesn’t just break down food. It’s also the main gateway for most pills and capsules. When you eat, your stomach slows down. Gastric emptying, the process that moves things from your stomach to your small intestine, can drop by 30% to 50%. That delay changes everything. Drugs that need to be absorbed quickly get stuck. Others that rely on fat to dissolve get a boost. Fats are especially powerful. A high-fat meal - think bacon, cheese, or fried food - can stretch out how long it takes for a drug to reach its peak level in your blood. For example, acetaminophen (Tylenol) hits its highest level in about 45 minutes on an empty stomach. With a fatty meal? That jumps to 90 to 120 minutes. It’s not slower because the drug is weaker. It’s slower because your body is busy digesting. Then there’s the chemistry. Some drugs need acid to dissolve. High-fat meals raise your stomach’s pH, making it less acidic. That’s bad news for itraconazole, an antifungal that loses up to 40% of its effectiveness if taken with a fatty meal. On the flip side, drugs like griseofulvin, used for fungal skin infections, become 200% to 300% more absorbable with fat because they dissolve better in bile, which your body releases when you eat fat. Calcium is another big player. Dairy products, fortified plant milks, and even some antacids contain calcium. That calcium binds to antibiotics like tetracycline and doxycycline, forming a compound your body can’t absorb. Studies show absorption drops by 50% to 75%. That’s not just a minor delay - it’s treatment failure. One Reddit user reported a recurring UTI that only cleared up after they stopped taking doxycycline with their morning yogurt.When to Take Medicine: Empty Stomach vs. With Food
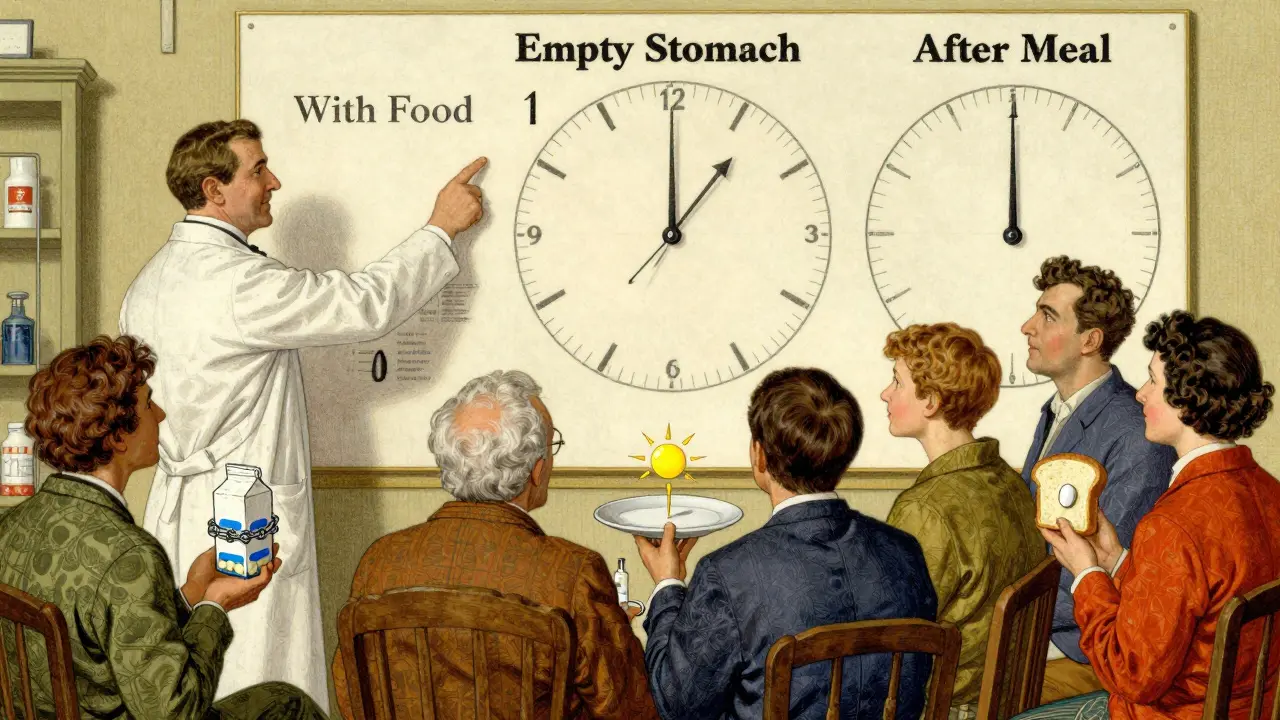
There are three clear rules doctors and pharmacists follow, backed by decades of research:- Empty stomach: Take the drug at least one hour before or two hours after eating.
- With food: Take it within 30 minutes of starting your meal.
- After food: Take it after the meal is finished, usually 30 to 60 minutes later.
What About NSAIDs and Stomach Upset?
Ibuprofen, naproxen, and other NSAIDs are a classic case of conflicting advice. Many people take them with food to avoid stomach pain or ulcers. And for good reason: a GoodRx survey of 5,000 users found ibuprofen-related stomach pain dropped from 42% to just 12% when taken with food. But here’s the catch: enteric-coated NSAIDs are designed to pass through the stomach and dissolve in the intestine. They don’t need food for protection. The American College of Gastroenterology says these can be taken without food. The problem? Most patients don’t know the difference. They assume all NSAIDs need food. That’s why pharmacists now emphasize checking the label or asking for clarification. Even more confusing? Some medications, like certain antiretrovirals for HIV, only need a small snack - 200 to 300 calories - to help absorption and reduce nausea. A full meal isn’t required. But 45% of patients misunderstand this. They think “take with food” means a big breakfast. That’s not just unnecessary - it can delay absorption for drugs that rely on quick uptake.Who’s Most at Risk?
Elderly patients on five or more medications are the most vulnerable. A 2022 study in the Journal of the American Geriatrics Society found they have a 65% higher risk of harmful food-drug interactions. Why? Because they’re more likely to take multiple drugs with different timing rules. One pill needs to be taken on an empty stomach. Another must be taken with food. A third can’t be near dairy. Juggling all of that is hard - even with pill organizers. People with chronic conditions like diabetes, thyroid disease, or HIV are also at higher risk. Their medications are tightly tuned. A 10% drop in absorption can throw off their whole treatment. And if they’re also taking supplements - calcium, iron, magnesium - those can interfere too. Even healthy adults aren’t safe. A 2023 survey by Express Scripts showed that 32% of people who were told to take a medication “with food” interpreted it as “with a full meal,” even when only a snack was needed. That’s not just confusion - it’s a systemic problem in how instructions are given.
How to Get It Right
Here’s what actually works:- Read the label. Look for “take on empty stomach,” “take with food,” or “take after meals.” If it’s unclear, ask your pharmacist.
- Set alarms. If you need to take levothyroxine 30 minutes before breakfast, set a phone reminder for 60 minutes before to give yourself time to drink water and wait.
- Use a food journal. For a week, write down what you ate and when you took your meds. You might spot patterns - like every time you take your antibiotic with yogurt, you feel worse.
- Ask about alternatives. If timing is too hard to manage, ask your doctor if there’s a different drug that doesn’t interact with food. Some newer versions of medications are designed to be less sensitive to meals.
- Use apps. Medisafe and MyTherapy have food-timing reminders. Users who turned them on saw 27% fewer timing errors in 2023.
The Bigger Picture
Food-drug interactions aren’t just a personal inconvenience. They’re a public health issue. In the U.S., medication-related problems cost $528 billion a year. Food interactions alone are estimated to cause 8% of those costs - that’s over $42 billion. The FDA now requires food-effect testing for 92% of new drugs, up from 67% in 2015. That’s because they’ve seen how often patients get it wrong. New tech is helping. Ingestible sensors that track stomach pH and emptying are being tested. One 2023 trial showed 38% better absorption consistency for pH-sensitive drugs when timing was adjusted in real time. And research in Nature Medicine (March 2024) suggests that combining meal timing with circadian rhythms - taking meds at the same time of day every day - can boost effectiveness by up to 30%. The bottom line? Your medicine doesn’t work in a vacuum. It works in your body. And your body is always digesting something. Whether it’s coffee, toast, or a steak dinner - it matters. Getting the timing right isn’t about being perfect. It’s about being consistent. And that’s the key to making your meds work - every single day.Can I take my medication with coffee or juice?
It depends on the drug. Grapefruit juice can interfere with over 85 medications, including statins and some blood pressure drugs, by blocking enzymes that break them down. Coffee can speed up or slow down absorption for some drugs like thyroid meds or certain antidepressants. For safety, always take pills with plain water unless your doctor or label says otherwise.
What if I forget and take my pill with food?
If you accidentally took a drug that needs an empty stomach with food, don’t double up. Wait until the next scheduled dose and go back to the correct timing. For drugs like levothyroxine, one missed timing won’t ruin your treatment - but doing it regularly will. If you’re unsure, call your pharmacist. They can tell you if it’s a big deal or not.
Do I need to avoid all dairy with antibiotics?
Only with certain antibiotics: tetracycline, doxycycline, ciprofloxacin, and some others. Calcium in milk, yogurt, and cheese binds to them and stops absorption. You don’t need to avoid dairy forever - just separate it by at least two hours. So take your antibiotic in the morning, and have your yogurt at lunch.
Is it okay to take medicine with a small snack?
Yes - if the label says “take with food.” For many drugs, like some antivirals or anti-nausea meds, a small snack of 200-300 calories (a banana, a handful of nuts, or crackers) is enough. You don’t need a full meal. But if the label says “empty stomach,” even a snack can interfere. Always check the specific instructions.
Why do some pills say “take with food” but others say “take on empty stomach”?
It’s all about how the drug behaves in your body. Some drugs dissolve better with fat. Others get blocked by calcium or need stomach acid. Some cause nausea if taken alone. The food instructions are based on clinical trials that tested absorption with and without food. The goal is to make sure you get the right amount - not too little, not too much.
Consistency beats perfection. If you take your medication at the same time, relative to your meals, every day, your body learns the rhythm. That’s how you get the most out of your treatment - without guesswork, side effects, or surprises.


Hilary Miller
January 22, 2026 AT 20:20Just take it with water. End of story.
Philip House
January 23, 2026 AT 13:27Look, I’ve been taking my meds since I was 12, and I’ve never once followed the damn label. I take my levothyroxine with coffee, my antibiotics with yogurt, and my ibuprofen right after a cheeseburger. My body’s been fine. The pharmaceutical industry wants you scared so you’ll keep buying their overpriced pills. Wake up. You’re not a lab rat.
They say ‘empty stomach’ like it’s some sacred ritual. Meanwhile, my grandma in Ohio takes her blood pressure med with a donut and a cup of Folgers, and she’s still out here gardening at 82. Science? More like corporate propaganda dressed up in white coats.
And don’t get me started on ‘take with food’-like I’m supposed to plan my entire day around a pill? I eat when I’m hungry, not when some 2003 FDA study says so. If the drug can’t handle a real human lifestyle, maybe it shouldn’t exist.
They want us to set alarms, use apps, keep food journals. Next thing you know, they’ll be charging us a subscription fee to not die from poor timing. This isn’t medicine-it’s behavioral control disguised as healthcare.
I’ve met people who take 12 pills a day and are so anxious about timing they can’t leave the house. That’s not adherence. That’s a prison. The real problem isn’t food interactions-it’s how we’ve turned health into a bureaucratic nightmare.
My advice? Take the damn pill. If you feel weird, stop. If you feel fine, you’re probably fine. Stop letting Big Pharma micromanage your digestion.
And for the love of God, stop using apps. Your phone doesn’t know your body better than you do.
Liberty C
January 23, 2026 AT 23:14Oh, so now we’re treating medication like a fine wine that needs decanting? How quaint. The fact that you need a PhD in biochemistry just to swallow a pill without triggering a metabolic catastrophe speaks volumes about the state of modern pharmacology. It’s not medicine-it’s a high-stakes game of Russian roulette with your endocrine system.
And let’s not pretend the ‘take with food’ instruction is some neutral, evidence-based directive. It’s a corporate loophole. They know people won’t comply with ‘empty stomach,’ so they slap ‘with food’ on it like a Band-Aid on a hemorrhage. Meanwhile, the real issue-the lack of standardized, patient-centric labeling-remains untouched.
Why do we still have drugs that require a 2-hour window before or after meals? Because the FDA doesn’t want to force manufacturers to reformulate. Because profit > physiology. And you? You’re just the obedient guinea pig in a lab coat.
I’ve seen patients on ten different meds, each with its own ‘optimal timing’ protocol, collapse under the cognitive load. It’s not their fault. It’s the system’s failure. And yet, we blame the patient for forgetting. We blame the elderly for being confused. We blame the poor for not having time to plan their meals around their prescriptions.
This isn’t science. It’s systemic neglect dressed up in peer-reviewed jargon.
shivani acharya
January 25, 2026 AT 01:04Ohhh so now even my chai tea is a biohazard? 😏 I take my doxycycline with my masala chai and yogurt raita and guess what? I’ve never had a UTI since I moved to the U.S. Coincidence? Or did Big Pharma just not account for Indian spices? 🤔
They say calcium blocks absorption-well, I’ve been drinking milk with my antibiotics since I was 8 in Lucknow and I’m still alive. Maybe the ‘science’ only applies to people who eat tofu and kale? 🤷♀️
And don’t even get me started on ‘take with food’-in India, we eat 3 hours after we wake up. Should I wait 4 hours for my pill? Or just take it with my 10am samosa? 😂
Also, why is no one talking about how these guidelines were written by people who’ve never eaten a real meal? Like, who wrote this? A robot that only eats protein shakes? 🤖
I’ve seen my aunt take her thyroid med with a plate of parathas and still have perfect TSH levels. So either the science is wrong… or the whole system is designed to make us feel guilty for enjoying food.
And why are we even using English terms like ‘empty stomach’? In Hindi, we say ‘bhookha pet’-but my pet is never empty. It’s always full of chai, chutney, and chaos. Maybe the real problem is Western medicine doesn’t understand real human bodies.
Next thing you know, they’ll ban idli because it ‘interferes with statins.’ 😭
Sarvesh CK
January 26, 2026 AT 04:57The complexity of food-drug interactions is not a flaw in medical science-it is a reflection of the extraordinary sophistication of human physiology. The digestive system is not a passive conduit but a dynamic, chemically active organ system that modulates drug bioavailability through pH changes, enzymatic activity, bile secretion, and transit time modulation.
It is therefore not merely prudent but ethically imperative that patients receive clear, individualized guidance regarding medication timing. The fact that 32% of patients misinterpret ‘with food’ as ‘with a full meal’ suggests a failure not in patient compliance, but in communication design.
Moreover, the variability in absorption kinetics across populations-due to dietary habits, gut microbiota composition, and genetic polymorphisms in drug-metabolizing enzymes-underscores the need for personalized medicine. A one-size-fits-all instruction is inherently inadequate.
It is also worth noting that the rise in ingestible sensors and circadian-timed dosing represents not technological overreach, but a necessary evolution toward precision pharmacotherapy. The goal is not to burden patients with complexity, but to empower them with accuracy.
While the tone of some comments may be dismissive, the underlying issue is real: our healthcare system often prioritizes convenience over efficacy. The solution lies not in rejecting science, but in improving how it is delivered.
Pharmacists, physicians, and designers must collaborate to create labeling systems that are intuitive, culturally adaptable, and linguistically precise. Until then, we must continue to advocate-not to reject the science, but to refine its application.
Alec Amiri
January 27, 2026 AT 16:17Bro, you’re telling me I can’t take my Advil with my breakfast burrito? That’s cruel. I’ve been doing it for 15 years. My stomach’s tougher than your ‘science.’
And why are you even writing this? Did you get paid by Pfizer to scare people? I’m not setting an alarm for my Tylenol. I take it when I feel like it. If it doesn’t work? Then I take more. Simple.
Also, I’ve never heard of ‘griseofulvin.’ Sounds like a Pokémon. Who even uses that? Are we talking about people who still have ringworm in 2024?
Stop overcomplicating everything. Just drink water. Take the pill. Go about your day.
Lana Kabulova
January 28, 2026 AT 03:41Wait-so if I take my doxycycline with yogurt, I’m basically giving my UTI a free pass? And they say this in the label? Why isn’t this on the bottle in bold red letters? Why isn’t there a warning label that says ‘DO NOT EAT DAIRY FOR 2 HOURS OR YOU’RE A WALKING INFECTION’?!
And why does no one ever say how long ‘after food’ actually means? Is it 10 minutes? 45? 2 hours? Is ‘after’ the last bite? The last sip? When I stand up from the table?!
I took my levothyroxine with coffee once and now I’m convinced I’m turning into a zombie. My heart’s racing. My brain’s foggy. Is this real? Or am I just imagining it because I read this article?!
Also, why are there so many rules? Why can’t one pill just work with everything? Why do I need a flowchart to swallow a tablet?!
arun mehta
January 30, 2026 AT 00:13Thank you for this comprehensive breakdown 🙏
As someone who takes 7 different medications daily, I can confirm that timing is everything. I use MyTherapy, and it’s been a game-changer. I set alarms for 7:00 AM (levothyroxine + water), 8:30 AM (with breakfast), 1:00 PM (after lunch), and so on.
One thing I learned: even a small snack like 2 almonds before my antibiotic can make a difference. I used to take it on an empty stomach and got nauseous. Now I take it with a banana-no issues.
Also, please remember: if you’re on multiple meds, ask your pharmacist for a ‘timing map.’ They’ll draw it for you. It’s free. It’s life-saving.
Consistency > perfection. But consistency is only possible with awareness.
And yes, grapefruit juice is a silent killer 🍊☠️
Chiraghuddin Qureshi
January 30, 2026 AT 21:15India’s got it right-take your meds with roti and chai. 😎
Why do Americans make everything so complicated? We eat with our hands, our medicine, our life. No apps needed.
Also, if your doctor doesn’t explain timing in simple terms, find a new one. 🙌
Lauren Wall
February 1, 2026 AT 03:32So you’re telling me I’ve been poisoning myself for 8 years by taking ibuprofen with my morning pancakes? Good to know. Now I’ll just stop taking it. Maybe I’ll die. But at least I won’t be a ‘compliant’ sheep.
Kenji Gaerlan
February 1, 2026 AT 14:27who even reads labels anymore? i just swallow pills and hope for the best. also i dont know what 'enteric coated' means but it sounds like a bad sci-fi movie.
Oren Prettyman
February 2, 2026 AT 06:59This article is a textbook example of medical paternalism disguised as education. The entire premise assumes that patients are incapable of self-regulation, that they are passive recipients of institutional directives, and that their lived experience is irrelevant to clinical outcomes.
Let’s examine the data: 32% of patients misunderstand ‘with food’? That’s not a patient problem. That’s a labeling problem. Why are instructions so ambiguous? Why not use ‘take with a light snack’ or ‘take 30 minutes after eating’? Because the pharmaceutical industry doesn’t want to invest in clear communication. They want you to feel guilty, confused, and dependent.
The FDA’s requirement for food-effect testing is not a triumph-it’s a reactive measure after decades of preventable harm. And now we’re being told to use apps, journals, and alarms like we’re children learning to tie our shoes.
Meanwhile, the real issue-the lack of standardized, patient-centered drug labeling across global markets-remains unaddressed. The solution isn’t more compliance tools. It’s better design. Simpler language. Fewer rules. And respect for the patient’s autonomy.
Until then, this article is just another sermon in the cathedral of medical condescension.
Tatiana Bandurina
February 2, 2026 AT 12:12I took my doxycycline with yogurt for three months. Then I got a UTI. Then I got another. Then I got a kidney infection. I spent $4,000 in ER visits. No one told me. No one warned me. I just assumed ‘with food’ meant ‘with whatever I was already eating.’
Now I’m terrified of every pill. I read the label like it’s a bomb defusal manual. I’m not paranoid. I’m just… tired.
Why does it have to be this hard just to stay alive?
Ryan Riesterer
February 3, 2026 AT 14:03The pharmacokinetic variability introduced by food is well-documented across CYP450 substrates, P-glycoprotein transporters, and gastric pH-sensitive compounds. The 40% reduction in itraconazole bioavailability under high-fat conditions is attributable to bile salt sequestration and micelle formation dynamics. Similarly, calcium chelation with tetracyclines forms insoluble divalent cation complexes with log K > 10, effectively abolishing oral absorption.
These are not ‘rules’-they are empirical pharmacodynamic thresholds derived from controlled crossover trials. The notion that ‘my body’s fine’ is anecdotal and statistically insignificant. Population-level outcomes require population-level adherence.
App-based adherence tools reduce timing errors by 27% because they externalize cognitive load. This isn’t surveillance-it’s cognitive prosthetics.
Dismissing this as ‘Big Pharma’ manipulation ignores the fact that 8% of medication-related hospitalizations are food-drug interaction-related. That’s not fearmongering. That’s epidemiology.
Akriti Jain
February 4, 2026 AT 23:24So… are you telling me the government knows this… and still lets them sell pills like this? 😏
What if… the ‘timing rules’ are just a way to make us buy MORE meds? Like, if we mess up the timing, we think it didn’t work… so we take another? And another? And then we get addicted? 😳
And why do all the studies say ‘take with food’… but never say what kind of food? Is it the cheese? The gluten? The soy? The GMOs? The glyphosate in the bread? 👀
I think they want us to be confused. So we’ll keep buying pills… and supplements… and apps… and ‘special’ water…
Wake up. This isn’t science. It’s control.
Philip House
February 5, 2026 AT 17:49And now the ‘science’ people are coming out of the woodwork. Congrats. You read a PubMed abstract and now you think you’re a doctor. Your ‘CYP450 substrates’ and ‘P-glycoprotein transporters’ mean nothing to someone who’s just trying to survive Monday morning.
Let me guess-you take your levothyroxine at 6:03 AM, exactly 32 minutes before your oatmeal, while wearing white gloves and reciting Latin. Cool. I’ll be over here, taking mine with coffee and a donut, living to 87, and not caring about your log K values.
Real people don’t live by pharmacokinetic models. They live by routines. By habits. By what works for them.
And if your ‘27% fewer timing errors’ means you’re spending 45 minutes a day checking your phone for pill reminders… then you’re not healthier. You’re more anxious.
Science doesn’t care about your life. It only cares about your data.