Why Temperature and Humidity Matter for Your Medications
Think about your insulin, antibiotics, or birth control pills sitting on a windowsill or in a bathroom cabinet. That’s not just a bad habit-it’s a risk to your health. Medications aren’t like canned soup or cereal. They’re complex chemical formulas designed to work within tight environmental limits. If the temperature climbs too high or the air gets too damp, those drugs can break down, lose strength, or even turn harmful. The temperature and humidity control for safe medication storage isn’t optional-it’s a science-backed requirement that keeps your pills effective and your body safe.
The U.S. Food and Drug Administration (FDA) found that in 2022, nearly 8 out of 10 drug recalls were tied to temperature problems during storage or shipping. That’s not a glitch. That’s a pattern. And it’s happening in homes, pharmacies, and hospitals alike. The World Health Organization estimates that 15-20% of all medications worldwide are wasted because they were stored wrong. That’s $35 billion gone-money, medicine, and lives on the line.
What Are the Right Temperature Zones for Medications?
Not all drugs need the same conditions. The U.S. Pharmacopeia (USP) breaks storage into four clear categories:
- Room Temperature Storage: 20°C to 25°C (68°F to 77°F). This is the sweet spot for most pills, capsules, and tablets. You’re allowed brief excursions between 15°C and 30°C (59°F to 86°F), but don’t make it a habit.
- Controlled Cold Storage: 2°C to 8°C (36°F to 46°F). This is for insulin, some vaccines, biologics, and certain injectables. Your fridge isn’t just for milk-it’s a medical device for these drugs.
- Frozen Storage: -25°C to -10°C (-13°F to 14°F). Used for specific biologics and long-term storage of certain compounds. Never freeze anything unless the label says so.
- Deep Frozen Storage: Below -20°C (-4°F). Reserved for highly sensitive products like some gene therapies or rare specialty drugs.
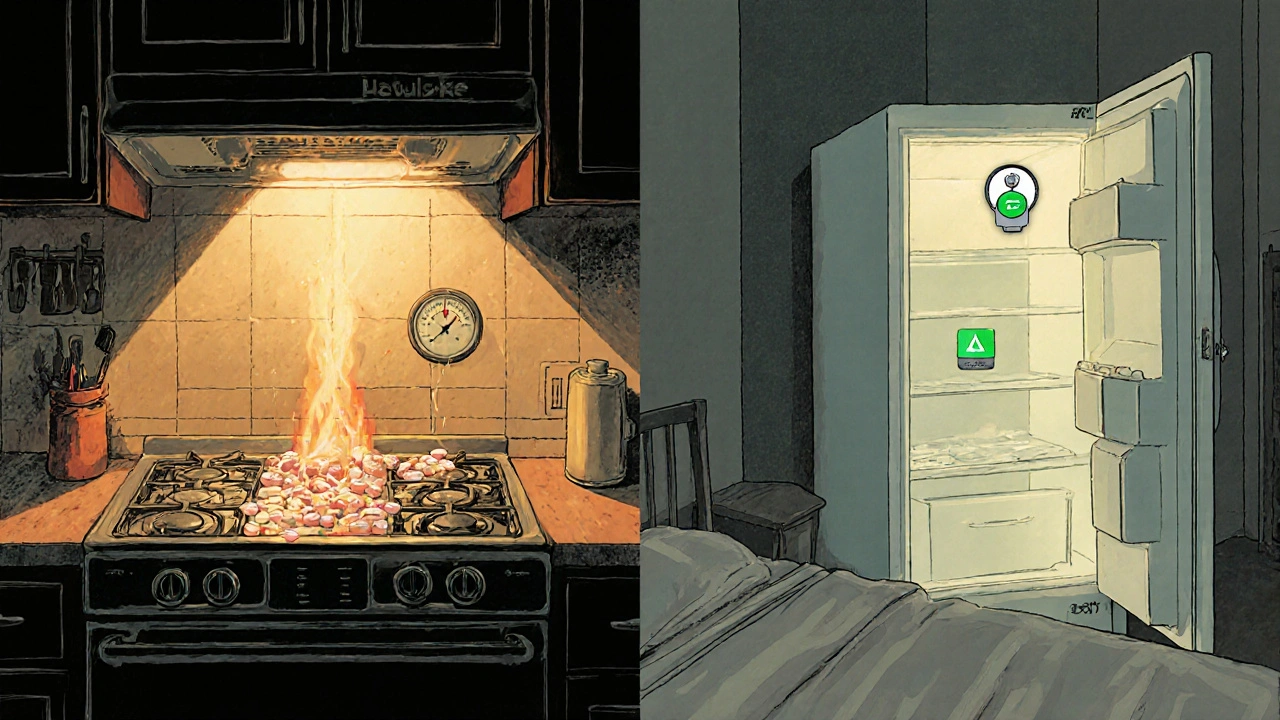
Here’s the catch: many people think “room temperature” means anywhere in the house. It doesn’t. A kitchen near the oven, a garage in summer, or a car parked in the sun can hit 40°C (104°F)-way above the safe limit. Even a bathroom with a hot shower can push humidity above 70%, which ruins moisture-sensitive drugs like nitroglycerin or certain antibiotics.
Humidity: The Silent Killer of Medications
Temperature gets all the attention, but humidity is just as dangerous. Most medications are designed to stay dry. Too much moisture causes pills to swell, crumble, or degrade chemically. The WHO and USP both recommend keeping relative humidity around 50%. That’s not a suggestion-it’s a target.
Why does this matter? Look at hormone-based drugs: birth control, thyroid meds, chemotherapy agents. A 2022 study from Baystate Health showed these drugs lost 23-37% of their potency after just a few days in high humidity. That’s not a little less effective. That’s a treatment that might not work at all. And if you’re taking it for epilepsy or heart conditions, that’s life-threatening.
And don’t assume your medicine cabinet is dry. Bathrooms are the worst place for storage. Showers, sinks, and steam turn them into mini saunas. Even a closet near a washing machine can get damp. Store your meds in a cool, dry drawer-not a humid bathroom.
Where NOT to Store Your Medications
Common storage spots are dangerous. Here’s what to avoid:
- Bathrooms: Steam from showers raises humidity. Even if it’s not hot, the moisture breaks down pills.
- Kitchens: Ovens, stoves, and dishwashers create heat spikes. A cabinet above the fridge? That’s a hot zone.
- Windowsills: Sunlight heats up glass and can trigger chemical reactions. UV light degrades some drugs faster than heat.
- Car glove boxes: In summer, temperatures inside a car can hit 60°C (140°F). That’s enough to melt capsules and ruin tablets.
- Refrigerator doors: Every time you open the door, the temperature swings. That’s why vaccines are stored in the center-not the door.
The CDC and American Society of Health-System Pharmacists (ASHP) both recommend storing medications in a central, interior closet or drawer-away from heat, light, and moisture. A bedroom drawer is often the safest bet.
Monitoring Equipment: It’s Not Optional
If you’re storing insulin, vaccines, or other temperature-sensitive drugs, you need a data logger. Not just a thermometer you check once a week. A buffered data logger that records temperature every 30 minutes, has an alarm if it goes out of range, and comes with a current calibration certificate.
Why? Because door openings, power outages, or faulty fridges can cause excursions you never notice. Dickson Data’s 2023 analysis of 15,000 pharmacy logs found that 18.7% of facilities had at least one temperature spike above 77°F during summer-with an average duration of over 4 hours. That’s long enough to ruin a vial of insulin.
Even in homes, cheap digital thermometers are unreliable. They don’t buffer the probe, so they spike when the door opens and give false readings. You need a device that smooths out those fluctuations. Look for models with low-battery alerts, min/max tracking, and ±1°F accuracy. They cost $50-$100. That’s less than one prescription refill.
Temperature Strata: Why Your Fridge Lies to You
Here’s something most people don’t know: your refrigerator isn’t uniform. Helmer Scientific’s 2022 study showed a 3.5°C (6.3°F) difference between the top shelf and the bottom. The door? Even worse-temperature swings there are 2.8°C (5°F) higher than the center.
That’s why vaccines and insulin must be stored in the center of the fridge, not on the door or against the back wall. The back wall can get too cold and freeze the medication. The door gets warm every time you open it. The center? That’s the most stable spot.
Same goes for storage units in pharmacies or clinics. If you’re not mapping the temperature across all shelves and corners, you’re guessing. The WHO now requires temperature mapping for all storage areas-meaning you have to test multiple points over 24-48 hours to prove the space is truly stable.
Training and Compliance: It’s Not Just About the Equipment
Having a data logger won’t help if no one knows what to do when it beeps. A 2023 ASHP report found that facilities with formal staff training reduced temperature excursions by 63%. That’s huge.
Training includes:
- How to read the logger’s min/max readings
- What to do when an alarm sounds (immediate action, not “I’ll check tomorrow”)
- How to document and report incidents
- When to quarantine affected meds
And it’s not just pharmacies. Home caregivers, nursing homes, and even patients themselves need to understand this. The Joint Commission found that 62% of pharmacy deficiencies in 2022 were tied to improper storage of sterile supplies-and most of those were due to staff not knowing the rules.
What’s Changing in 2025 and Beyond
Regulations are tightening. In January 2024, the FDA announced new rules: by December 2025, all healthcare facilities must use real-time remote monitoring for temperature-sensitive medications. That means your fridge or storage unit will send alerts to a central system-no more manual logs.
USP is also updating Chapter 1079 to require tighter humidity control: 45% ± 5% for moisture-sensitive drugs. And AI is stepping in. Companies like Polygon Group have tested AI systems that predict temperature spikes before they happen-cutting excursions by 76% in trials.
Meanwhile, the global cold chain market is booming. It’s expected to hit $38.4 billion by 2030. Why? Because the cost of getting it wrong is too high. The WHO says half of all vaccines are wasted globally due to temperature failures. That’s $20 billion lost-and millions of people left unprotected.
What You Can Do Today
You don’t need a fancy lab to keep your meds safe. Here’s your simple checklist:
- Read the label. If it says “store in refrigerator,” put it in the center-not the door.
- Buy a buffered data logger ($50-$100). Set it to log every 30 minutes. Check the alarm settings.
- Store meds in a dry, dark, interior drawer. No bathrooms. No kitchens. No windows.
- Check your fridge’s temperature weekly. It should be between 2°C and 8°C (36°F-46°F).
- If you see a temperature spike, don’t guess-call your pharmacist. Ask: “Is this medication still safe?”
- Train anyone who handles your meds: family, caregivers, nurses.
Medications are precision tools. They’re not meant to survive in a hot car or a steamy bathroom. The science is clear. The stakes are high. And the solutions? Simple, affordable, and life-saving.
Frequently Asked Questions
Can I store my insulin in the freezer?
No. Freezing insulin destroys its structure. Even if it looks normal after thawing, it may not work properly. Insulin should only be stored in the refrigerator at 2°C to 8°C (36°F-46°F). Unopened insulin can be kept at room temperature for up to 28 days, but never freeze it.
What if my medication gets too hot during shipping?
If your medication arrives warm-especially if it’s insulin, vaccines, or hormones-don’t use it. Contact your pharmacy immediately. Many pharmacies will replace it at no cost. Temperature excursions during shipping are common, but you’re not responsible for the risk. Always check the packaging for signs of heat damage: melted pills, discolored liquids, or swollen containers.
Are over-the-counter meds affected by temperature?
Yes. Even aspirin, antacids, and cough syrup can degrade. Aspirin breaks down into vinegar-like compounds when exposed to heat and humidity, reducing its effectiveness. Liquid antibiotics may grow bacteria if stored too warm. Always follow the storage instructions on the label-even for OTC drugs.
How do I know if my medication has gone bad?
Look for changes: pills that crumble, tablets that change color, liquids that become cloudy or separate, or capsules that leak. Smell matters too-some meds develop a vinegar or chemical odor when degraded. If you’re unsure, don’t take it. Bring it to your pharmacist. They can test it or advise if it’s still safe.
Do I need a special fridge for my medications?
Not necessarily. A standard refrigerator works if it’s reliable and you store meds in the center, away from the door and back wall. But if you’re storing multiple temperature-sensitive drugs, consider a dedicated medical fridge. These maintain tighter control, have alarms, and don’t get opened as often. Home medical supply companies sell them for under $300.


swatantra kumar
November 20, 2025 AT 22:06Matthew McCraney
November 22, 2025 AT 11:34Rebecca Cosenza
November 22, 2025 AT 12:47Rusty Thomas
November 23, 2025 AT 15:53Brianna Groleau
November 24, 2025 AT 12:00serge jane
November 24, 2025 AT 20:19Sarah Swiatek
November 26, 2025 AT 13:22Dave Wooldridge
November 26, 2025 AT 22:18