When you take CBD, a non-intoxicating compound from cannabis that’s used for pain, anxiety, and sleep. Also known as cannabidiol, it doesn’t get you high—but it can change how your body handles other medicines. That’s because CBD interacts with a group of liver enzymes called CYP450 enzymes, a family of proteins responsible for breaking down over 60% of all prescription drugs. These enzymes are like the body’s cleanup crew for medications. When CBD shows up, it can slow them down—or sometimes speed them up—changing how fast your body processes things like blood pressure pills, antidepressants, or even painkillers.
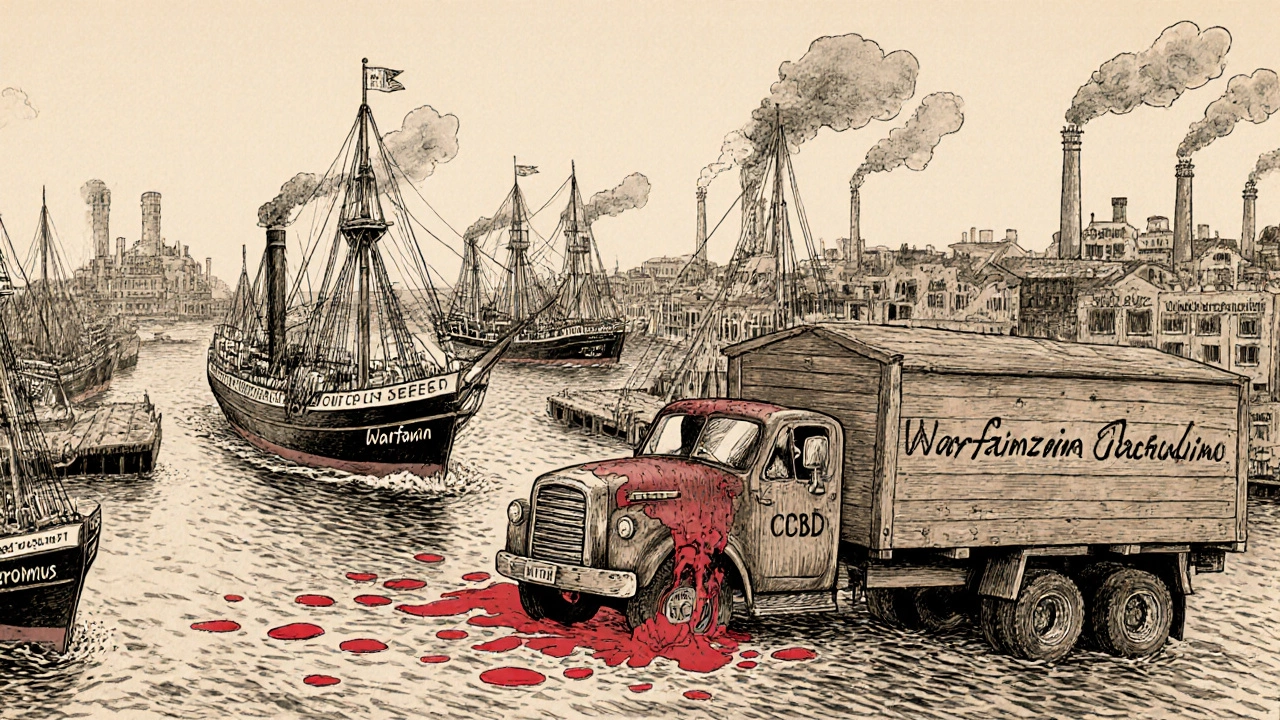
This isn’t theoretical. People taking CBD alongside warfarin, a blood thinner that requires precise dosing to avoid dangerous bleeding have seen their INR levels spike. Others on clobazam, an anti-seizure drug used for epilepsy, reported stronger side effects when adding CBD, because the enzyme that breaks down clobazam got blocked. Even common OTC meds like ibuprofen or statins can be affected. The same enzymes that handle CBD also handle drugs for cholesterol, depression, seizures, and heart conditions. If you’re on any regular medication, CBD isn’t just a harmless supplement—it’s a potential wildcard.
It’s not all bad news. Some people use CBD specifically because it slows down metabolism of certain drugs, letting them take lower doses. But guessing isn’t safe. Dosing matters. Timing matters. And your liver’s capacity matters. That’s why the posts below dive into real cases: how CBD affects kidney meds, what happens when you mix it with antidepressants, and which supplements are safest to combine. You’ll find clear comparisons, patient experiences, and practical steps to avoid dangerous interactions. Whether you’re using CBD for sleep, pain, or anxiety, you need to know how it plays with your other meds. The answers aren’t in marketing claims—they’re in the science, and they’re right here.