When your kidneys aren’t filtering fluids properly, diuretics for kidney disease, medications that help the body get rid of extra fluid through urine. Also known as water pills, they’re one of the most common tools doctors use to ease swelling, lower blood pressure, and reduce strain on failing kidneys. But not all diuretics are created equal—some can actually hurt your kidneys if used wrong.
There are three main types: loop diuretics, stronger drugs like furosemide that act fast on the loop of Henle in the kidney, thiazide diuretics, milder options like hydrochlorothiazide that work lower down in the kidney, and potassium-sparing diuretics, drugs like spironolactone that help keep potassium levels stable. For chronic kidney disease, loop diuretics are usually the first choice because they work even when kidney function is low. Thiazides lose effectiveness as kidney damage gets worse. And potassium-sparing diuretics? They’re useful—but only if your potassium levels are monitored closely. Too much potassium can be dangerous, especially with kidney disease.
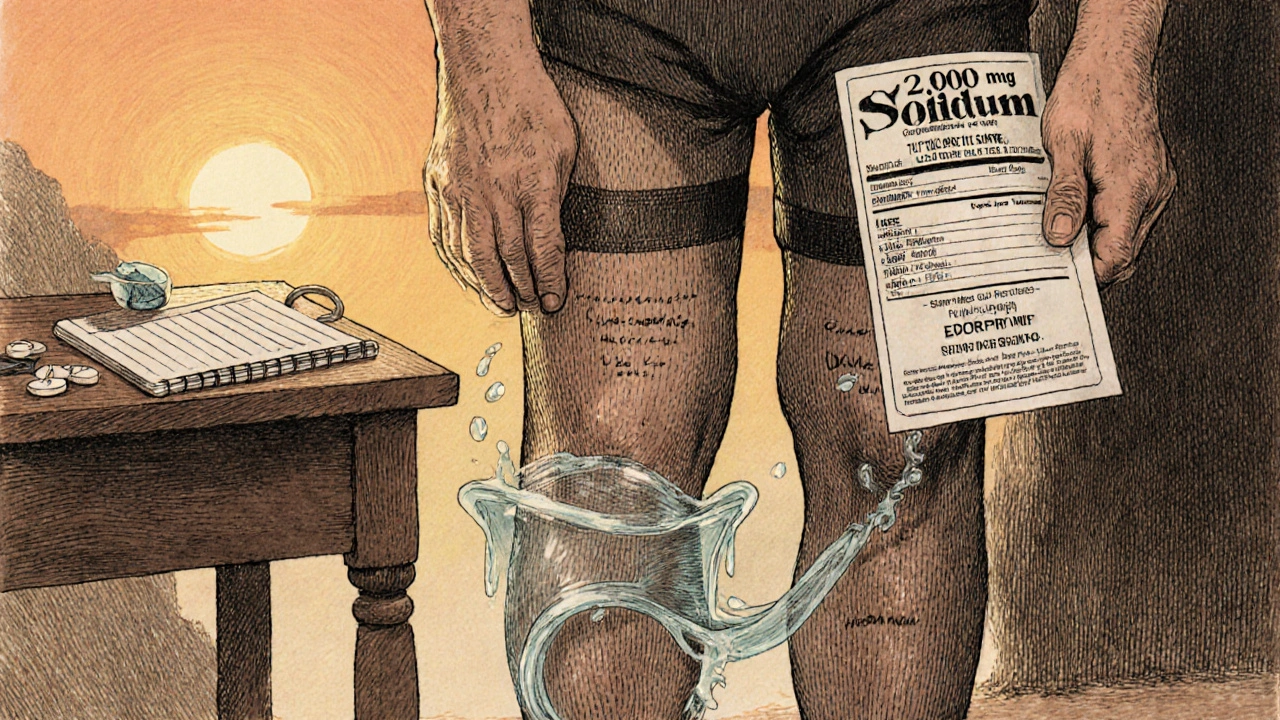
Many people think diuretics are just for swelling, but they’re also part of managing high blood pressure—a major cause of kidney damage. Taking them the wrong way—skipping doses, overdoing it, or mixing them with NSAIDs like ibuprofen—can crash your blood pressure or make kidney function worse. That’s why doctors don’t just prescribe them and walk away. They check your labs, watch your weight, and adjust doses based on how you’re doing.
What you’ll find in the posts below isn’t just a list of drugs. It’s real-world insight on how diuretics connect to other kidney treatments, what alternatives exist, and how they interact with common meds like allopurinol or blood pressure pills. You’ll see how some patients benefit from combining diuretics with lifestyle changes, while others need to switch because of side effects. No fluff. Just what matters when your kidneys are under stress.