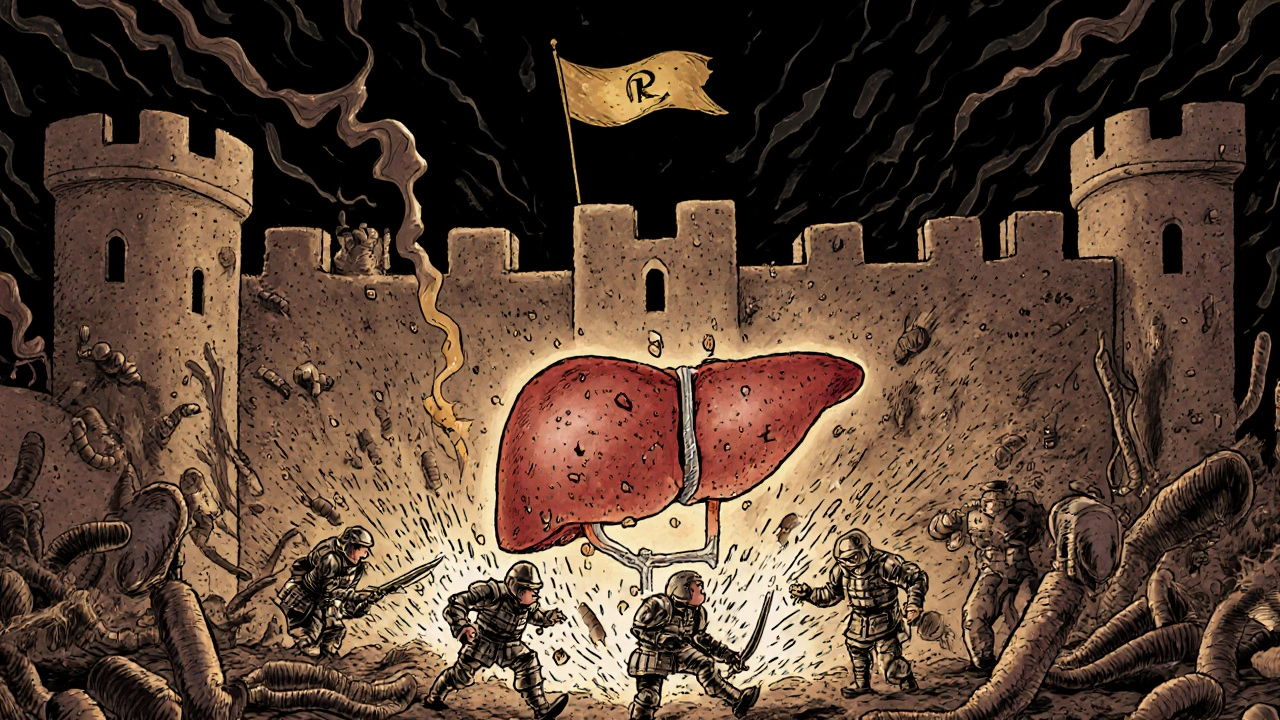
When you take an antibiotic, a medicine used to treat bacterial infections. Also known as antibacterial agents, they save lives—but they can also harm your liver without warning. Liver damage from antibiotics isn’t rare. It’s one of the most common causes of drug-induced liver injury, liver harm caused by medications, not viruses or alcohol. You might feel fine, take your pills exactly as prescribed, and still end up with elevated liver enzymes. No one warns you about this until it’s too late.
Some antibiotics are riskier than others. Lincocin (lincomycin), an older antibiotic used for serious infections. has been linked to liver stress, especially in people with existing conditions. Others like amoxicillin-clavulanate, erythromycin, and sulfonamides show up often in reports of liver toxicity. It’s not always about dosage—it’s about your body’s reaction. One person takes amoxicillin with no issue. Another ends up in the hospital with jaundice. There’s no perfect way to predict who’s at risk, but certain factors raise the odds: age over 55, long-term use, alcohol use, or having other liver conditions like fatty liver or hepatitis.
Most people don’t realize their liver is under attack because symptoms are sneaky. You might just feel tired, lose your appetite, or get mild nausea. Dark urine, yellow eyes, or itchy skin? Those are red flags. Blood tests catch it early—ALT and AST levels rising, bilirubin climbing. But if you skip follow-ups because you feel okay, you’re playing Russian roulette with your liver. Post-marketing data shows these reactions often show up months after starting treatment, long after doctors assume you’re safe. That’s why medication safety, the ongoing monitoring of how drugs affect people after approval. matters more than ever. Clinical trials miss rare side effects. Real-world use doesn’t.
Not all antibiotics are equal. Some are safer for your liver than others. If you’ve had liver issues before, ask your doctor about alternatives. Don’t assume generics are always the same—some formulations trigger reactions others don’t. And never combine antibiotics with alcohol, herbal supplements like kava or green tea extract, or other drugs that stress the liver, like statins or acetaminophen. The combination can turn a mild problem into a crisis.
What you’ll find below are real stories, real data, and real guidance from posts that dug into the details. From how doctors spot liver damage after the fact, to which antibiotics are most likely to cause trouble, to what blood tests actually mean—you’ll see how this isn’t just theory. It’s something that happens to real people, often without warning. And you deserve to know how to protect yourself before it’s too late.